**PLEASE NOTE- THIS IS A RE-PRINT OF DR. VANDEN BOSSCHE’S ARTICLE WHICH WAS ONLY MADE AVAILABLE TO ME VIA PDF AND IS NOT ON HIS WEBSITE YET. HE GAVE ME PERMISSION TO SHARE. PLEASE GO TO
voiceforscienceandsolidarity.org FOR MORE OF HIS WORK.
Poor virus-neutralizing capacity in highly C-19 vaccinated populations could soon lead to a fulminant spread of Sars-CoV-2 super variants that are highly infectious and highly virulent in vaccinees while being fully resistant to all existing and future spike-based C- 19 vaccines
Table of content
➢ Key message
➢ Introduction
➢ Summary
➢ Why this call?
➢ Why is Omicron not the long hoped for end station of this pandemic?
➢ What does the official ‘expert’ narrative tell us?
➢ What does the epidemiology of the current pandemic teach us?
➢ Why should we care about lack of herd immunity when infections in vaccinees barely cause any severe disease, let alone death?
- There isn’t even any hope that the current epidemiological situation could lead to herd immunity any time soon
- There are increasing signs of more generalized immune suppression in vaccinees as indicated by a steadily growing number of reports rising incidences of other respiratory illnesses, other viral diseases and even cancer.
- There is substantial evidence that Omicron is enabling a highly vaccinated population to exert immune pressure on its pathogenicity
➢ What does the host immune response to viral infectivity teach us about the evolutionary dynamics of SC-2 in the ongoing pandemic?
➢ Is there a causal relationship between the enhanced susceptibility of vaccinees to infection and their diminished susceptibility to disease?
- Poor neutralization capacity results in enhanced susceptibility to ADEI
- Poor neutralization capacity results in diminished susceptibility to severe disease because diminished
trans infection capacity results in diminished trans fusion and, therefore, decreases the likelihood of
systemic/ severe disease
- Diminished trans infection capacity results in diminished trans fusion and, therefore, decreases the
likelihood of systemic/ severe disease
➢ Could (and if so, how?) SC-2 escape from immune pressure exerted on its conserved infection- enhancing NTD site while simultaneously outperforming Omicron in infectiousness?
Author: G. Vanden Bossche, DVM, PhD March 2022
1
➢ Is O-glycosylation of RBD feasible and would it provide a logical approach for shielding the conserved enhancing NTD site without compromising enhanced viral infectiousness?
➢ Why would O-glycosylation be more likely than N-glycosylation?
➢ Could O-glycosite mutants decouple enhanced viral infectiousness from diminished pathogenicity in
vaccinees by enabling trans fusion?
➢ How could O-linked glycosylation promote viral virulence in vaccinees?
➢ Could O-linked glycosylation also allow for resistance to the C-19 vaccines and, therefore, provide for a high level of viral infectiousness in vaccinees?
➢ What would be the consequences of site-specific O-glycosylation on the phenotypic characteristics of the virus?
➢ How would the O-glycosylated Newco variants evolve in a highly vaccinated population and what would be their impact on individual and public health?
➢ How long will it take for more pathogenic SC-2 variants to become dominant?
➢ In healthy non-vaccinated individuals, O-glycosylated Newcos will only cause asymptomatic to mild
disease
➢ Why are C-19 vaccinated people no longer able to rely on relevant innate immune cells when circulating variants become resistant to the neutralizing capacity of the vaccinal Abs?
➢ Lessons from Nature
➢ Why would vaccination with a live (attenuated) virus at the beginning of this pandemic (i.e., in an
immunologically naïve population) not have had the same catastrophic prognosis?
➢ How should a pandemic of an acute, self-limiting viral infection be monitored from a public health viewpoint?
➢ Conclusion
➢ Figures 1-7
➢ Attachment:
I. About glycosylation of SC-2
II. About O-glycosylation of SC-2
III. About the role of C-type lectins in the pathobiology of SC-2 infection
Author: G. Vanden Bossche, DVM, PhD March 2022
2
List of abbreviations
Ab: Antibody
ACE2: Angiotensin-converting enzyme 2
ADED: Ab-Dependent Enhancement of Disease
ADEI: Ab-Dependent Enhancement of Infection
ADII: Ab-Dependent Inhibition of Infection
CoV: Coronavirus
DC-SIGN: Dendritic cell-specific intercellular adhesion molecule-3-Grabbing Non-integrin
L-SIGN: Liver/ Lymph node-specific intercellular adhesion molecule-3-grabbing non-integrin
LRT: lower respiratory tract
(S)-NTD: N-terminal domain on spike protein
(S)-RBD: Receptor-binding domain on spike protein
(S)-RBM: Receptor-binding motif on spike protein (i.e., the region on the RBD that is in direct contact and interacts with the ACE2 receptor on target host cells)
S: spike protein
SC-2: SARS-CoV-2 virus
SIGLEC1: Sialic acid–binding immunoglobulin-like lectin 1 URT: upper respiratory tract
Author: G. Vanden Bossche, DVM, PhD
March 2022
3
Definitions
Depending on their relative concentration and the type of presentation of S to permissive cells (i.e., presentation on free-moving virions - as is typically the case in the URT - as opposed to presentation on virions attached to host DCs or target cells in the LRT), Abs with different specificities (i.e., directed at the RBD or the receptor-binding motif [RBM] within the RBD, or directed at variable or conserved epitopes within NTD) may have a distinct impact on viral infectious behavior and could either neutralize or enhance viral infectivity.
Neutralizing anti-RBM Abs, for example, will promote inhibition of infection of cells expressing high levels of ACE2 (typically prevailing in the URT) by free SC-2 virions (via Ab-mediated hindrance of ACE2- dependent viral entry), thereby hampering infection in the URT; these Abs will also promote trans fusion between SC-2-infected cells and uninfected target cells in the LRT or distant organs (i.e., via Ab- mediated enhancement of ACE2-independent, fusogenic rearrangement of cell surface-expressed S), thereby enabling ‘trans fusion’ to promote systemic C-19 disease. Non-neutralizing, non-enhancing anti-NTD Abs would use the same mechanism to promote ACE2-independent trans fusion between SC- 2-infected cells and uninfected target cells in the LRT.
In contrast, non-neutralizing enhancing anti-NTD Abs will promote infection of cells expressing high levels of ACE2 (typically prevailing in the URT) by free SC-2 virions (via Ab-mediated enhancement of ACE2-dependent viral entry), thereby enhancing infection in the URT; the very same Abs will hamper trans infection between virus-loaded, migrating DCs and uninfected target cells in the LRT or distant organs (i.e., via Ab-mediated hindrance of ACE2-independent, fusogenic rearrangement of S expressed on virions that are tethered to the surface of migrating DCs), thereby preventing ‘trans infection’ to promote systemic C-19 disease.
This already explains why a spectacular decrease in the neutralizing capacity of vaccinal Abs (e.g., as a result of Omicron’s resistance to the vaccine) is driving Ab-dependent enhancement of infection (ADEI) while reducing the incidence of severe disease.
Definition of trans infection: Trans infection relates to a productive infection of target cells by SC-2 virions that are carried on the surface of DCs and which is triggered by binding of S surface-expressed N- linked glycans to C-type lectin receptors expressed on the surface of DCs in a way that promotes exposure of a polypeptide domain within NTD that is capable of binding to sialogangliosides comprised within lipid rafts of target cell membranes. This interaction would enable fusogenic rearrangement of spike protein and hence, facilitate attachment of the RBM to the ACE2 receptor.
Definition of trans fusion: Transfusion relates to ACE2-independent cell-to-cell fusion between a SC-2- infected and a non-infected neighboring cell, thereby resulting in the formation of syncytia and promoting cell-to-cell spread of infection in the target organ.
Author: G. Vanden Bossche, DVM, PhD March 2022
4
Poor virus-neutralizing capacity in highly C-19 vaccinated populations could soon lead to a fulminant spread of Sars-CoV-2 super variants that are highly infectious and highly virulent in vaccinees while being fully resistant to all existing and future spike-based C- 19 vaccines
Key message
I SERIOUSLY expect that a series of new highly virulent and highly infectious SARS-CoV-2 (SC-2) variants will now rapidly and independently emerge in highly vaccinated countries all over the world and that they will soon spread at high pace. I expect the current pattern of repetitive infections and relatively mild disease in vaccinees to soon aggravate and be replaced by severe disease and death.
Unfortunately, there is no way vaccinees can rely on assistance from their innate immune system to protect against coronaviruses1 as their relevant2 innate IgM antibodies are increasingly being outcompeted by infection-enhancing vaccinal Abs, which are continuously recalled due to the circulation of highly infectious Omicron variants. In contrast, Omicron’s high infectiousness would enable the non- vaccinated to train their innate immune defense against SC-2 while the infectious and pathogenic capacity of the new SC-2 variants would be debilitated in the non-vaccinated for lack of infection- enhancing Abs in their blood. Unless we immediately implement large scale antiviral prophylaxis campaigns in highly vaccinated countries, there shall be no doubt that the pandemic will end by taking a huge toll on human lives.
Introduction
‘More infectious’ variants have been reported to break through protection against infection conferred by vaccine-induced neutralizing Abs. Although vaccinees have now become more susceptible to infection, their vaccinal Abs still largely protect them from severe disease. However, cases of hospitalization in fully vaccinated people are now increasingly reported in some highly vaccinated countries (e.g., UK, Israel, South-Korea). This could indicate that some new variants are now breaking through protection (against severe disease) conferred by the C-19 vaccines and that it may only be a matter of time before additional mutations are incorporated that allow a more virulent variant to replace Omicron. The evolutionary dynamics of this pandemic are highly suspicious of mass vaccination shifting the course of a natural pandemic by promoting the expansion in prevalence of more infectious immune escape variants. It would be important to be able to verify whether and how population-level immune pressure induced by this large-scale immunization program could explain the current clinical and epidemiological observations as this knowledge could subsequently be used to predict the upcoming consequences of this human intervention on both individual and public health. The aim, therefore, of the present work is to predict
1 and most likely also against several other glycosylated enveloped viruses or other glycosylated components expressed at the surface of infected or otherwise pathologically altered cells
2 ‘relevant’ relates to the fact that I am departing from the assumption that – although polyspecific – not all innate Abs will recognize CoV (including all types of SC-2 variants)
Author: G. Vanden Bossche, DVM, PhD March 2022
5
the potential biological implications of the ongoing C-19 mass vaccination program with an as high as possible level of certainty. The present paper probably stands as the first reported attempt to confronting my own multidisciplinary insights with relevant references from the literature to scientifically analyze and explain the putative pathophysiologic mechanisms underlying the mysterious evolution of the ongoing C- 19 pandemic. The scientific approach used has been based upon deductive reasoning and there is probably no better way of validating the conclusions of this work than citing Sherlock-Holmes:
“How often have I said to you that when you have eliminated the impossible, whatever remains, however improbable, must be the truth?”
As a result, a theory has been developed that is not only consistent with the current clinical and epidemiological observations but which is also supported by many scientifically validated principles. This theory is now translating in very concerning predictions about the potential implications of the ongoing C-19 mass vaccination program on both, individual and public health. As the conclusions make perfect scientific sense, its predictive value should be taken extremely seriously.
Summary
It cannot be denied that breakthrough infections with more infectious variants, including Omicron, have occurred as a result of vaccine-induced population-level immune pressure on spike protein (S)-specific neutralizing epitopes.
It has been established that non-neutralizing antibodies (Abs) directed at epitopes comprised within the conserved ‘enhancing’ site within the N-terminal domain (NTD) of S (S-NTD) not only contribute to Omicron’s enhanced infectiousness in vaccinees but are also likely to mitigate disease as the course of Omicron infections is rather mild. As Omicron is highly infectious, individuals are now at risk of rapid re- exposure to the virus. It follows that highly vaccinated populations are now placing more and more immune pressure on the infection-enhancing site within the S-NTD to prevent Omicron from causing systemic disease. I posit that this immune pressure is now at risk of driving natural selection of new SC-2 variants (‘Newco variants’) that will be endowed with one or more O-glycosylation sites that can shield the conserved NTD region comprising the non-neutralizing enhancing epitopes and thereby escape the disease-mitigating effect exerted by the enhancing anti-NTD Abs in vaccinees. Hence, natural selection of mutations enabling more extensive O-glycosylation of spike protein would not only make Newco variants fully resistant to all potentially neutralizing vaccine-induced Abs directed at spike protein (S), and thereby enable an even higher level of viral infectiousness, but also render these new immune escape variants more virulent for vaccinees. As site-specific O-glycosylation of S would abrogate Ab- mediated protection against severe disease in vaccinees, Ab-dependent enhancement of viral infectiousness (ADEI) would now directly translate into Ab-dependent enhancement of C-19 disease (ADED). This would ultimately result in a tsunami of hospitalizations and deaths in highly vaccinated populations whereas the unvaccinated would be better and better protected against the Newco variants thanks to their ‘enhanced’ (i.e., trained) innate immunity and because of reduced infectiousness and trans infectiousness of the virus in the upper and lower respiratory tract, respectively.
Author: G. Vanden Bossche, DVM, PhD March 2022
6
As glycosylation of viral proteins responsible for initiation of infection are well known to evolve as a result of immune pressure on the viral life cycle, there is a high need for molecular epidemiology surveillance of SC-2 to not only monitor evolutionary changes in viral peptide sequences but to also perform glycosylation profiling and glycoproteomics of SC-2 spike protein (S).
No ongoing pandemic can be tamed by vaccines that mitigate symptoms but cannot provide sterilizing immunity. At this stage, the only way to avert a large-scale disaster is to immediately replace the mass vaccination program by large scale antiviral chemoprophylaxis campaigns in highly vaccinated countries.
Why this call?
I know this is a bad time to share my deep concerns about the future evolution of this pandemic. I know the world is currently getting more than enough of very concerning news; in addition, scary predictions about the future evolution of this pandemic are never welcome. The only reason why I nevertheless continue to express my concerns is that I cannot refrain from urging national and international public health agencies to immediately engage their populations in large scale antiviral chemoprophylactic campaigns, especially in highly vaccinated countries. Given the high infectivity rate that characterizes the spread of Omicron, the rather ‘mild’ course of infections we are currently witnessing cannot be considered the endgame prelude of this pandemic.
Even if the mass vaccination program were immediately halted, a spectacular and immediate reduction of viral infection rates in highly vaccinated populations would be required to prevent these populations from further exerting spike (S)-directed immune pressure on Omicron. Based on the analysis of molecular epidemiologists, there can be no doubt that convergent evolution of SC-2 towards protection of its life cycle from host immune attacks will continue for as long as these attacks will threaten the life cycle of the virus but not in ways that can fully prevent its replication and transmission. Because of strong selective immune pressure on viral infectiousness, the virus has already turned to expansion in prevalence of highly infectious variants as a mechanism to ensure its survival and to escape new immune attacks. As will be explained below, the evolution of SC-2 towards more virulent circulating variants directly results from the combination of its resistance to potentially neutralizing vaccinal Abs and the high level of infectiousness it achieves in highly vaccinated populations. It is, therefore, paramount that we stop mass vaccination and immediately reduce the infection rate in the population.
Why is Omicron not the long hoped for end station of this pandemic?
Already at the beginning of 2021, molecular epidemiologists reported that population-level immune pressure on spike protein (S) is a major driver of immune escape mutations and that once these mutations start to accumulate, it’s basically just a matter of time before they recombine in constellations with unpredictable properties that will survive and thrive, provided they manage to resist the immune pressure exerted by the population (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7941658/pdf/nihpp-2021.02.23.21252268v3.pdf). Although none of these scientists dares to mention mass vaccination as an obvious cause of population-
Author: G. Vanden Bossche, DVM, PhD March 2022
7
level immune pressure placed on S, it cannot be denied that large scale vaccination of largely immunologically SC-2 naïve populations during the C-19 pandemic has forced these populations to exert extensive immune pressure on viral infectiousness as C-19 vaccines are directed at S, which is responsible for viral infectiousness (https://trialsitenews.com/why-is-the-ongoing-mass-vaccination- experiment-driving-a-rapid-evolutionary-response-of-sars-cov-2/). It can’t be denied either that massive population-level immune pressure has led to the enhanced dominance of vaccine-resistant3 viral variants (e.g., belonging to the Omicron ‘family’). Given that a pandemic can only be ended by reducing the likelihood of viral transmission, massive circulation of a virus in populations that have now become highly susceptible to viral infection (i.e., because of high vaccination rates) is certainly not a situation that is favorable to ending this pandemic.
What does the official ‘expert’ narrative tell us?
Despite all biological evidence, including Darwinian theory, global and public health officials and advising experts have continued to dismiss serious warnings of myself and others that the evolutionary dynamics of this pandemic may largely be shaped by the mass vaccination program they have been advocating for all along. But now that the virus (i.e., Omicron) has become largely resistant to the vaccine-induced neutralizing Abs, even some independent scientists tend to believe that C-19 vaccinations have contributed to reducing the severity of this pandemic and that we’re now shifting to a ‘natural’ mass immunization mode that is even better because it uses a highly infectious but overwhelmingly mild virus (i.e., Omicron). Omicron would, therefore, serve as an almost perfect ‘live attenuated vaccine’! Stakeholders of this thoughtless vaccination program are now claiming that we owe this ‘blessing’ to the success of this very program. Anyway, many scientists now seem to believe that - thanks to Omicron - the population managed to open a window of opportunity for establishing herd immunity and, therefore, to end the pandemic!
What does the epidemiology of the current pandemic teach us?
There are currently several observations in highly vaccinated populations that are suspicious of suppression of the innate immune system in most of the population (i.e., vaccinees) in that they are pointing to enhanced susceptibility of the vaccinees to infection instead of diminished susceptibility, which would be expected if herd immunity were growing. Extension of the mass vaccination program to very young and poorly antigen-experienced children will only enlarge the reservoir of vulnerable individuals and cause additional vaccine breakthrough surges in this age group.
Because of the high level of Omicron’s infectiousness in highly vaccinated populations, the frequency of infections occurring at any given time has dramatically increased. It is important, though, to note that the number of ‘cases’ is no longer a reliable metric for the infection rate in the population as cases now almost exclusively relate to cases of C-19 disease. As the decline in hospitalization and death rates have
3 For the purpose of this report, ‘vaccine-resistant’ refers to the capacity of SC-2 to resist potentially virus- neutralizing Abs in vaccinees
Author: G. Vanden Bossche, DVM, PhD March 2022
8
now led governments and public health authorities to largely lift the public health measures and as many ‘cases’ are now going unreported because infections are mostly characterized by relatively mild symptoms (both in the unvaccinated and vaccinated part of the population), the overall number of cases
4 - as reported by the official national and international databases - is certainly largely underestimated .
Nevertheless, many countries are still reporting overall infection rates that are relatively high. This observation together with the moderate decline that follows a peak of cases and/or the rapid succession of individual waves that are only separated by short intervals and/or failure of the case rate curves to rejoin the baseline in-between two waves, are all signs of the population’s enhanced susceptibility to infection (see fig. 1). So, if the vaccines would perform as well as our natural immune defense during a natural pandemic, we would expect most people to develop asymptomatic infection (instead of mild or moderate disease) and that after each of a limited number of waves, the infection rate sharply declines to rejoin the baseline (instead of leveling off prematurely before temporarily transitioning into a kind of plateau or irregular pattern of smaller waves). However, high waves of infectiousness are no longer a guarantee of a spectacular subsequent decline of cases. It seems, therefore, that the fluctuation in the case rates is merely reflecting changes in the susceptibility to infection in different parts of the population with no evidence of capacity being built to provide sterilizing immunity. This is what is now causing ‘herd susceptibility’ instead of ‘herd immunity’. The more the mass vaccination campaigns are now involving younger and younger age groups, the more the reservoir of susceptible people is growing and the more surges will likely be grafted on the new baseline, the level of which has already been raised following waves of more infectious variants. It has been reported that vaccinees are, indeed, more susceptible to infection but that this enhanced susceptibility does not translate in more (cases of) severe disease (https://www.medrxiv.org/content/10.1101/2022.01.28.22270044v1). It seems, therefore, as if the vaccine is responsible for promoting the vaccinee’s susceptibility to infection while hampering progression of infection to severe disease. This is in sharp contrast to the course of a natural pandemic in an unvaccinated population, in which waves of infection are associated with a substantial surge in morbidity and mortality, typically in the most vulnerable part of the population. These surges are typically followed by a dramatic reduction of the infection rate and it typically only takes a few waves for a natural pandemic to transition into endemicity as this is what it takes to protect the remaining vulnerable part of the population by herd immunity.
Based on the evolutionary dynamics of the current pandemic and the fact that the above-described trends are most obvious in highly vaccinated populations, it is tempting to postulate that the overall population (the majority of which consists of vaccinees) exerts immune pressure on the virus such as to reduce the severity of C-19 disease while enabling a high level of susceptibility to infection. It is highly unlikely that the combination of these 2 characteristics would be pure coincidence. It is more likely that they have a common denominator which is to be sought in the large-scale immune intervention on the population. As the altered phenotypic characteristics of the virus in highly vaccinated populations involve enhanced viral infectiousness, it seems likely that the anti-spike immune response is involved. Given the evidence of increasing resistance of Omicron to potentially neutralizing Abs and the combined observation of enhanced viral infectiousness with diminished severity of disease, it seems already
4 Many ‘cases’ are now going unreported as infections are mostly characterized by relatively mild symptoms; those are now less frequently reported and testing frequency, especially in vaccinees, has been largely down-scaled. Diminished reporting of disease cases also implies diminished contact tracing.
Author: G. Vanden Bossche, DVM, PhD March 2022
9
obvious that the current evolutionary dynamics of this pandemic may now be explained by the interaction between the virus (Omicron) and non-neutralizing vaccinal Abs (see further below).
Why should we care about lack of herd immunity when infections in vaccinees barely cause any severe disease, let alone death?
A word of caution needs to be said about this naïve question. Whereas Omicron might rather benefit the unvaccinated part of the population, in which repeated exposure to this highly infectious variant is training the innate immune response, this virus is likely to behave very differently in the vaccinated part of the population.
As usual, the devil is in the detail and the detail is often about getting down to the nitty-gritty of the evolutionary dynamics of the interplay between the virus and the host immune system. As this interplay has been profoundly disturbed by thoughtless human intervention, it seems completely counterintuitive that the relatively low hospitalization and mortality rates are the consequence of herd immunity. As already mentioned above, infection rates in highly vaccinated countries are still high (and likely largely underestimated due to the overwhelming mildness of Omicron disease in vaccinees and in most of the non-vaccinated age groups) and thus, there is currently no sign of herd immunity.
- There isn’t even any hope that the current epidemiological situation could lead to herd immunity any time soon:
Omicron is known to largely resist potentially neutralizing Abs elicited by the current C-19 vaccines. Diminished neutralization capacity of vaccinal Abs has been shown to substantially increase the affinity of non-neutralizing vaccinal Abs for the N-terminal domain of S (S-NTD) [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8351274/pdf/main.pdf]. In a previous contribution of mine (https://trialsitenews.com/will-omicron-induce-herd-immunity-or-will-it-enable-sars-cov-2-to- transition-into-variants-capable-of-potentiating-ade-in-vaccinees/), I’ve already suggested that these non-neutralizing vaccinal Abs compete with relevant multi-specific innate Abs (i.e., IgMs) for binding to SC-2 as in both cases binding is thought to involve multivalent binding interactions (
Since innate immune effector cells (IgM-secreting B1a cells) can recognize self-motifs displayed on surface-expressed N-glycan patterns (such as displayed on the surface of glycosylated enveloped viruses, including coronaviruses), innate IgM Abs are thought to mediate cytotoxic killing (via NK cells) of virus-infected target cells at an early stage of infection and thereby contribute to sterilizing immunity. It has been shown that in case of asymptomatic infection, an increase of innate/ natural CoV-reactive IgM Abs and a high frequency of NK cells correlate with abrogation of infection and prevention of disease (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7772470/pdf/fimmu-11-610300.pdf).
Consequently, a high prevalence of elevated titers of non-neutralizing anti-S Abs (due to dominant
10
Author: G. Vanden Bossche, DVM, PhD March 2022
circulation of vaccine-resistant variants) is likely to suppress the capacity of highly vaccinated populations to curtail viral transmission and hence, to achieve herd immunity.
Suppression of relevant innate Abs could be particularly pronounced under the following circumstances:
1. In the case innate immune effector cells had no opportunity to adapt to viral exposure prior to being short-circuited by vaccinal S-specific Abs (e.g., in case of high-speed mass vaccination programs conducted in populations with relatively low infection rates). Because innate polyreactive IgM Abs produced by poorly trained B1a-derived immune effector cells will not have sufficient affinity to compete with the non-neutralizing anti-NTD Abs for binding to the virus. This would particularly be the case when viral exposure occurs shortly after the first vaccine shot5, which cannot be avoided when mass vaccination campaigns are conducted during a pandemic.
2. In the case of C-19 vaccination of children. Although present in high quantities, innate Abs in children
are largely naïve (i.e., antigen-inexperienced) and, therefore, prone to being outcompeted by S-specific
6
vaccinal Abs . A worst-case scenario could, therefore, consist of combining vaccination of young children
with public health measures that are at risk of substantially reducing their exposure to respiratory viral infections (e.g., because of masking, physical distancing and quarantine of healthy children who tested positive).
3. In the case of recent natural or C-19 vaccine-mediated boosting7 of vaccinees (or their re-vaccination with an updated C-19 vaccine that better matches the S protein on the circulating variant) or in the case of vaccination of subjects who previously recovered from C-19 disease. In all these cases, previously vaccine-induced Abs will be recalled. The recall will result in disproportionally high titers and/ or disproportionally high binding affinity of non-neutralizing anti-S Abs, which not only outcompete innate polyreactive IgMs but also enhance viral infectiousness (see further below). This implies that in countries with high vaccine coverage rates, vaccinees are now more susceptible to infection with the circulating
8
virus, which is likely to predominantly boost their infection enhancing anti-NTD Abs . Under these
circumstances, additional booster vaccinations are unlikely to change the impact of mass vaccination on population-level immunity and the course of the pandemic.
Consequently, there can be no doubt that the continuation of mass vaccination campaigns, which are now increasingly targeting children and focusing on booster shots (or Omicron-specific vaccinations),
5 This may already explain why during the 5 weeks after the first dose of vaccine was given, mortality rates in the vaccinated have been reported to be 20 times higher than in the unvaccinated. Especially the S-encoding genetic C-19 vaccines could lead to a strong stimulation of non-neutralizing anti-NTD Abs that have a disproportionally high binding affinity towards the conserved enhancing site on an antigenically mismatched spike on the circulating viral variant (i.e., not matching the antigenic constellation of the S encoded by the vaccine). This is because S produced by these genetic vaccines is known to stay in the body for several months. This would obviously lead to a prolonged stimulation of Abs, including those that are directed at the enhancing site on the antigenically mismatched variant.
6 It is important to note that subjects with naturally acquired Abs are endowed with trained innate immunity as acquisition of these Abs results from the virus breaking through the innate immune defense.
7 Especially the S-encoding genetic C-19 vaccines could lead to a strong recall of non-neutralizing anti-NTD Abs that have a disproportionally high binding affinity towards the conserved enhancing site of an antigenically mismatched spike on the circulating viral variant (for the same reason as explained under footnote 5 above)
Author: G. Vanden Bossche, DVM, PhD March 2022
11
will result in a significant loss of the population’s capacity to generate herd immunity.
- There are increasing signs of more generalized immune suppression in vaccinees as indicated by a steadily growing number of reports on rising incidences of other respiratory illnesses, other viral diseases and even cancer.
It is likely, but not yet unambiguously proven, that surges in those diseases are due to diminished recognition of self-like antigens, which is known to be a critical function of innate Abs. However, it is tempting to speculate that suppression of the functional activity of innate Abs that recognize surface- expressed self-like patterns of self-glycans are a direct consequence of innate immune suppression. This is certainly a field that needs to be further explored.
- There is substantial evidence that Omicron is enabling highly vaccinated populations to exert immune pressure on its pathogenicity
Anti-NTD Abs have been shown to trigger enhancement of infection (https://www.journalofinfection.com/article/S0163-4453(21)00392-3/fulltext;
A highly vaccinated population that continues to be exposed to a SC-2 variant that is largely resistant to neutralization by S-directed Abs will be featured by a steadily increasing prevalence of elevated anti- NTD Ab titers and, therefore, become increasingly susceptible to infection. It is reasonable to postulate that in vaccinees, who are boosted as a result of their exposure to Omicron, especially the infection
9
enhancing anti-NTD Abs will benefit from a strong recall effect . This would imply that even after having
contracted C-19 disease, vaccinees remain highly susceptible to infection while serving as an important source of selective (i.e., Omicron-specific) transmission. As more and more vaccinees will, therefore, become infected or re-infected, and given the fact that the vast majority of reported cases relate to mild disease and that there is reasonable evidence for assuming that anti-NTD Abs mediate protection from severe disease (https://www.nature.com/articles/s41586-021-03925-1.pdf), it is tempting to speculate that highly vaccinated populations are exerting substantial immune pressure on the conserved enhancing site of S-NTD to suppress progression of infection to severe disease. Since the advent of Omicron, registered cases rates - although largely underestimated – have substantially increased and even when waves decline, the average cases rates in highly vaccinated countries exceed those previously seen with other variants. This suggests that a substantial level of immune pressure on viral pathogenicity is maintained at a higher baseline value for a prolonged period of time. Although the protective effect of these Abs has been demonstrated in animal in vivo studies, there are currently no established assays allowing to measure the biological activity of these Abs in vitro. Consequently, it has not been possible to demonstrate that the prevalence of elevated titers of infection enhancing anti-NTD Abs in highly vaccinated countries is currently on the rise. However, if their prevalence is rising, there
9 The epitopes targeted by the enhancing Abs are conserved across different SC-2 variants and will provoke a strong recall effect, regardless of whether they are comprised within Omicron or within an S-based vaccine
Author: G. Vanden Bossche, DVM, PhD March 2022
12
should be a molecular mechanism that plausibly links enhanced infectiousness to reduced virulence and that clarifies why and how elevated, non-neutralizing Abs could place immune pressure on viral virulence. It is critical to elucidate this mechanism since it may allow to predict whether or not the evolutionary dynamics of this pandemic are currently paving the way for yet a more problematic immune escape variant to be selected and expand in prevalence. As the baseline of the curves depicting the ‘Omicron’ case rates has been raised in highly vaccinated countries, it is reasonable to predict that the valley of fitness to be crossed by a potential new variant will be shallower and, therefore, likely to reduce the fitness cost incurred. In other words, the lag time to the emergence of the next family of dominantly circulating immune escape variants would be expected to be much shorter.
A better insight in the immune pathobiology of the virus might even allow to assess the risk that new, more virulent, immune escape variants emerge and explore whether such variants would be able to pair enhanced virulence with a level of infectiousness that is high enough to rapidly outcompete Omicron (see below under: What does the science teach us about the evolutionary dynamics of SC-2 in the ongoing pandemic?).
After SC-2 has become very infectious in highly vaccinated populations and largely resistant to vaccine- induced neutralizing Abs (primarily directed at variable RBD epitopes), it would only need to overcome one additional immunological hurdle, i.e., resistance to vaccine-induced infection-enhancing Abs, as a prerequisite for being classified as a ‘Variant of High Consequence’. Due to its high level of infectiousness and virulence in vaccinees and its complete resistance to S-based vaccines, the spread of a such variant in highly vaccinated populations would have catastrophic consequences. The analysis proposed below should, therefore, be taken very seriously.
What does the host immune response to viral infectivity teach us about the evolutionary dynamics of SC-2 in the ongoing pandemic?
My understanding of the evolutionary dynamics of SC-2, the mechanism of its interaction with different types of anti-S Abs and the type of future mutations the virus is likely to incorporate in response to the immune pressure mounted by the population, are highly consistent with and to a large extent based on the findings of F.A. Lempp et al. (https://www.nature.com/articles/s41586-021-03925-1), H. Arase et al. (https://www.sciencedirect.com/science/article/pii/S0092867421006620) and the observations reported by the teams of N. Izquierdo-Useros (https://www.nature.com/articles/s41423-021-00794- 6.pdf), W.S. Barclay (https://www.biorxiv.org/content/10.1101/2021.12.31.474653v1), J. Fantini (https://pubmed.ncbi.nlm.nih.gov/34384810/), H. Wang (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7863934/#B233-ijms-22-00992) and K. Gupta (https://www.biorxiv.org/content/10.1101/2021.12.17.473248v2).
These researchers, together with several others referenced to in their publications, have already highlighted that anti-S Abs may inhibit or enhance viral infectiousness or disease, depending on the overall virus-neutralizing Ab titer as measured in vitro and the conformational structure of relevant Ab epitopes as determined by the context of S expression (i.e., expressed on free virions or on virions attached to DCs or on virus-infected host cells).
Author: G. Vanden Bossche, DVM, PhD March 2022
13
The mechanisms behind the interplay between population-level immune pressure and evolutionary immune escape strategies of SC-2 have been addressed in form of answers to several relevant questions:
Is there a causal relationship between the enhanced susceptibility of vaccinees to infection and their diminished susceptibility to disease?
The combination of enhanced susceptibility to infection and diminished susceptibility to disease does not typically occur during a natural viral pandemic of an acute self-limiting viral disease.
From what follows below, one can reasonably conclude that enhanced resistance to vaccine-induced neutralizing Abs is responsible for both enhanced susceptibility to infection and diminished susceptibility to disease in highly vaccinated populations.
Poor neutralization capacity results in enhanced susceptibility to ADEI (fig 2)
Definition of ADEI: Enhancement of viral infectiousness which is triggered by binding of non-neutralizing ‘infection-enhancing’ anti-NTD Abs to a conserved (i.e., common among SC-2 variants but not across CoVs in general) antigenic site within NTD in a way that promotes the ‘open’ conformation of the RBD, thereby enhancing the attachment of the receptor-binding motif (RBM) to the ACE2 receptor and facilitating viral entry into the target cell
In the upper respiratory tract (URT), non-neutralized SC-2 virions infect epithelial cells that have a high level of ACE2 expression or are captured by C-type lectins on tissue-resident DCs that will transfer infectious virions to the lower respiratory tract (LRT) or other distant organs (https://www.nature.com/articles/s41586-021-03925-1.pdf). Diminished virus neutralization capacity of specific Abs towards variable RBD epitopes promotes the affinity of a subset of non-neutralizing Abs for infection-enhancing epitopes that are comprised within a specific, conserved, non-glycosylated site on NTD (https://www.journalofinfection.com/article/S0163-4453(21)00392-3/fulltext;https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7128678/pdf/main.pdf). It is likely, but not unambiguously proven, that a disproportionally high binding of vaccine-induced, non-neutralizing Abs to the conserved, enhancing site on NTD is due to changes in the structural arrangement of this antigenic site as this site is known to be part of a flexible region that packs tightly against the RBD of the neighboring protomer and as the RBD has been reported to undergo a dramatic conformational change upon binding to RBD-directed neutralizing Abs (https://pubs.acs.org/doi/pdf/10.1021/acs.jpclett.0c01431;https://www.science.org/doi/pdf/10.1126/science.abb2507; https://www.nature.com/articles/s41586- 021-03925-1.pdf). Potentially broadly neutralizing NTD-specific Abs would preferably bind to their corresponding epitopes comprised within a single, specific conserved ‘supersite’ on the NTD when the RBD is stabilized in its ‘open’ conformation by neutralizing RBD-specific Abs whereas potentially broadly infection-enhancing NTD-specific Abs situated within the same supersite would preferably bind to their corresponding epitopes when the RBD is in its ‘closed’ conformation and hence, poorly bound by neutralizing anti-RBD Abs. This would suggest that the single, conserved, glycan-free NTD supersite of neutralization as reported by some authors (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7962585/pdf/main.pdf;
Author: G. Vanden Bossche, DVM, PhD March 2022
14
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8820657/pdf/nihpp-2022.02.01.478695v1.pdf) overlaps with the single, conserved, glycan-free NTD supersite of infection enhancement reported by other authors (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8142859/pdf/main.pdf) and that epitope recognition on NTD would largely depend on structural rearrangements induced by conformational changes in the RBD that are triggered by its binding to neutralizing Abs.
Binding of non-neutralizing Abs to infection-enhancing epitopes comprised within the specific, conserved domain within NTD is known to facilitate recognition of the ACE2 receptor by RBD and, therefore, to enhance ACE2-dependent viral entry into host target cells (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8142859/pdf/main.pdf). This phenomenon is called ‘Antibody-Dependent Enhancement of Infection’ (ADEI). It has convincingly been documented that enhancing Abs do not lead to enhancement of infection in case neutralizing Abs are at high levels (https://www.sciencedirect.com/science/article/pii/S0092867421006620; https://pubmed.ncbi.nlm.nih.gov/34384810/). It has, therefore, been postulated that non-neutralizing Abs are particularly at risk of enhancing infection when viral exposure occurs in the presence of significantly reduced virus-neutralizing Ab titers. The latter situation would particularly apply to breakthrough infections10, where viral exposure occurs shortly after the first vaccine shot or even in individuals who have been fully vaccinated but whose Abs do no longer effectively neutralize the virus for lack of effective recognition of the corresponding S epitopes on the circulating variant by the vaccinal Abs (i.e., in case of increasing resistance of the circulating virus to potentially neutralizing Abs induced by the vaccine). Hence, ADEI would explain why - in a context of Abs induced by the current C-19 vaccines - Omicron seems to be much more infectious in comparison to previous variants. Scientists have already warned against the risk of mass vaccination campaigns using a spike protein format that is different from the one expressed on circulating variants as they acknowledge the risk that enhancing Abs could be induced by vaccination (https://www.journalofinfection.com/article/S0163- 4453(21)00392-3/fulltext; https://www.sciencedirect.com/science/article/pii/S0092867421006620). Their concern seems even more pertinent in the light of strong suspicion that infection-enhancing anti- NTD Abs compete with innate polyreactive IgM for binding to S. This is particularly worrisome in the case of Omicron since the neutralizing capacity of the vaccinal Abs has become very poor and the likelihood of re-exposure very high. This combination is likely to strongly boost the vaccinal infection- enhancing anti-NTD Abs. This would not only further raise the susceptibility of vaccinees to infection but also further suppress training of their B1a-derived innate immune effector cells and thereby prevent relevant polyreactive IgM from acquiring higher affinity for the virus. Viral transmission can, therefore, no longer be mitigated, which will only contribute to causing a snowball effect in that it self-amplifies the occurrence of ADEI and hence, makes any hope for achieving herd immunity completely vanish (see fig. 3).
Poor neutralization capacity results in diminished susceptibility to severe disease because diminished trans infection capacity results in diminished trans fusion and, therefore, decreases the likelihood of systemic/ severe disease (see figs. 3 and 4).
10 A ‘breakthrough’ infection relates to an infection that occurs after vaccination or in a vaccinated person Author: G. Vanden Bossche, DVM, PhD March 2022
15
Definition of trans infection: Trans infection relates to a productive infection of target cells by SC-2 virions that are carried on the surface of DCs and which is triggered by binding of S surface-expressed N-linked glycans to C-type lectin receptors expressed on the surface of DCs in a way that promotes exposure of a polypeptide domain within NTD that is capable of binding to sialogangliosides comprised within lipid rafts of target cell membranes. This interaction would enable fusogenic rearrangement of spike protein and hence, facilitate attachment of the RBM to the ACE2 receptor.
Definition of trans fusion: Transfusion relates to ACE2-independent cell-to-cell fusion between a SC-2- infected and a non-infected neighboring cell, thereby resulting in the formation of syncytia and promoting cell-to-cell spread of infection in the target organ.
Infectious SC-2 virions that are not bound to S-specific Abs or innate, polyreactive Abs can be captured by tissue-resident DCs at the mucosal portal of viral entry. Activated DCs migrate and transport infectious virions to the LRT or other distant target tissues (https://www.nature.com/articles/s41586- 021-03925-1.pdf), in which they may trans infect epithelial cells in the LRT or other distant tissue cells and cause systemic disease due to fusion of infected and non-infected tissue cells (see below).
Strong binding of the N- glycosylation sites of S to DC surface-expressed C-type lectins is likely to promote stabilization of RBD in the closed position (a diagram of the closed position of RBD is provided in the left panel of fig. 5). On the other hand, this tethering may promote exposure of a large, mostly glycan-free surface at the tip of the NTD11 that has been shown to enable attachment of the virus to gangliosides comprised within lipid rafts on target cells that are endowed with low cell surface expression of ACE2 (which is a characteristic of epithelial cells in the lungs and in other distant target tissues) such as to facilitate contact with the ACE2 receptor and enable productive infection (https://www.journalofinfection.com/article/S0163-4453(21)00392-3/fulltext; https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7128678/pdf/main.pdf). By enabling close contact to these target cells, the ganglioside-binding domain on NTD may trigger fusogenic rearrangement of the S- RBD which would promote stabilization of the RBD in the open position and thereby allow S to engender productive trans infection. This would already explain why migratory DCs loaded with SC-2 virions facilitate trans infection of host target cells endowed with low expression of ACE2 (as predominantly present in the LRT) [https://www.nature.com/articles/s41586-021-03925-1.pdf].
However, strong binding of the N- glycosylation sites of S to DC surface-expressed C-type lectins is likely to dramatically reduce the effectiveness of the infection-enhancing anti-NTD Abs in triggering the induction of the ‘open’ RBD state when upon their binding to the conserved infection-enhancing site. The open state of the RBD (a diagram of the open position of RBD is provided in the right panel of fig. 5) is required to allow the virus to recognize ACE2 receptors and invade host cells with low expression of ACE2. This would already explain why monoclonal neutralizing Abs (i.e., selective for the open conformation of RBD) can no longer neutralize infectious SC-2 virions that are tethered to the surface of DCs (https://www.nature.com/articles/s41586-021-03925-1.pdf).
11 This domain (111–158) is fully conserved among clinical isolates
Author: G. Vanden Bossche, DVM, PhD March 2022
16
Even though binding of the enhancing anti-NTD Abs to their epitopes comprised within the specific supersite on NTD would fail to trigger the induction of the open RBD state when S is bound to DC surface-expressed lectins, it would certainly induce substantial structural rearrangements, not only in the recognized parts of NTD but also in non-recognized regions (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7953435/pdf/main.pdf). It is, therefore, reasonable to assume that under these conditions the ganglioside-binding domain on NTD is no longer be able to make close contact to target cells endowed with low cell surface expression of ACE2 (which is a characteristic of lung epithelial cells and epithelial cells in other distant target tissues) and, therefore, fails to trigger the fusogenic rearrangement of S-RBD that would enhance its stabilization in the open position and enable S to engender productive trans infection.
It seems therefore plausible that enhancing Ab-mediated inhibition of C-type lectin-facilitated, ACE2- dependent trans infection of SC-2 as observed in vitro (https://www.nature.com/articles/s41586-021- 03925-1.pdf) is due to structural rearrangements within the S-NTD.
Diminished trans infection capacity results in diminished trans fusion and, therefore, decreases the likelihood of systemic/ severe disease (see fig. 3).
The interaction between C-type lectins on the surface of neighboring epithelial cells in the LRT (in particular Siglec-1; https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7863934/; https://www.nature.com/articles/s41586-021-03925-1.pdf) and oligomannoyslated N-glycans on the surface of S could not only enable trans infection between epithelial pulmonary cells but also facilitate attachment of S expressed on infected cells to the surface of neighboring uninfected cells, regardless of their level of ACE2 expression. Subsequently, trans fusion between infected and non-infected cells can be facilitated by neutralizing Abs that - by virtue of their binding to RBD epitopes - enable fusogenic rearrangement of S and, thereby, promote fusion between cell membranes (https://www.nature.com/articles/s41586-021-03925-1.pdf). Fusogenic Abs have been reported to contribute to systemic spread and dissemination of the virus at a later stage of infection (https://www.nature.com/articles/s41586-021-03925-1.pdf). Alternatively, fusogenic rearrangement of S could also be facilitated by non-neutralizing Abs that are directed against antigenically variable NTD epitopes. It has, indeed, been reported that also anti-NTD epitopes that are directed at the conserved supersite can inhibit cell-to-cell fusion (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7962585/pdf/main.pdf). Although the mechanism of Ab-dependent enhancement of fusion between infected and non-infected target cells (with low ACE2 expression) has not been reported in detail, it seems reasonable to propose that binding of these Abs to their epitopes induces a conformational change that promotes exposure of the ganglioside-binding domain at the tip of the NTD to facilitate fusogenic rearrangement of S. Fusion between infected and non-infected cells results in the formation of syncytia which have been reported to correlate with C-19 disease severity (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7164771/pdf/main.pdf;https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7677597/pdf/main.pdf;https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7128866/pdf/main.pdf).
Author: G. Vanden Bossche, DVM, PhD March 2022
17
It follows that Ab-facilitated disease does not depend on whether Abs have neutralizing capacity but on whether they can trigger fusogenic rearrangement of S to promote fusion of S-expressing cells with uninfected neighboring cells. In the absence of fusogenic Abs, syncytia formation induced by Omicron S, for example, is poor despite containing mutations that enhance S cleavage (https://www.biorxiv.org/content/10.1101/2021.12.17.473248v2;https://www.biorxiv.org/content/10.1101/2021.12.31.474653v1.full.pdf).
The above-described effect of anti-NTD Abs is obviously very different from the one observed in cells with high expression levels of ACE2 (and hence, representative of epithelial cells in the URT). Here, disproportional binding of anti-NTD Abs to S is thought to enhance ACE2-mediated viral attachment and entry and, therefore, responsible for ADEI in vaccinated people (https://www.journalofinfection.com/article/S0163-4453(21)00392-3/fulltext).
Based on all the above, it is tempting to postulate that viral variants which largely resist neutralization by anti-spike Abs induced by the current C-19 vaccines (e.g., Omicron) have a diminished capacity to engage in trans infection and, therefore, seem less pathogenic than previous SC-2 variants. In other words, the pathogenic behavior of Omicron in vaccinees is (indirectly) attenuated by poor neutralization activity of their anti-RBD Abs, which directly results from Omicron’s resistance to the vaccine. As already mentioned, poor neutralization capacity of the anti-RBD Abs is thought to result in a disproportionally high binding of infection-enhancing NTD-specific Abs to S, which has been shown to enable inhibition of C-type lectin-mediated trans infection in cells that express low levels of ACE2 such as those found in distant target tissues (https://www.nature.com/articles/s41586-021-03925-1.pdf). As a result, highly vaccinated populations are currently exerting substantial immune pressure on a part of the N-terminal domain (NTD) of Omicron’s spike protein that is now increasingly recognized by vaccine-induced, infection-enhancing Abs that prevent dissemination of SC-2 in distant organs, including the LRT. In conclusion, it appears that the explosive spread of Omicron, combined with its relatively mild symptoms in the vast majority of the population (this is certainly very atypical for a natural viral pandemic of an acute self-limiting viral disease!), is driven by population-level immune pressure on the enhancing NTD site. This insight is of critical importance because it strongly suggests that SC-2 is already proceeding with natural selection of additional mutations. As I write this report, more and more cases of more severe disease in vaccinees are being reported. As described below, I suspect that SC-2 could overcome Ab-mediated immune pressure on trans infection by glycosite mutations at predictive O-glycosylation sites. One cannot rule out that more abundant glycosylation of the RBD is already occurring; in that regard, it would certainly be useful to make the (evolving?) glycosylation profiles of Omicron spike protein available.
‘Could (and if so, how?) SC-2 escape from immune pressure exerted on its conserved infection- enhancing NTD site while simultaneously outperforming Omicron in infectiousness?
In other words, is there any kind of mutation(s) that could simultaneously enhance viral virulence and viral infectiousness in vaccinees while not affecting immune recognition in individuals known to not
Author: G. Vanden Bossche, DVM, PhD March 2022
18
exert immune pressure on the virus, i.e., the unvaccinated12 ? This would already suggest a type of mutation that promotes ADEI (e.g., by conferring resistance to potentially neutralizing vaccinal anti-S Abs) while preventing the same enhancing Abs from blocking systemic disease. Knowing that Omicron infection in vaccinees is now intrinsically pairing enhanced infectiousness with mitigated disease symptoms, the question looks at first glance very challenging. However, on a background of extensive and prolonged suboptimal immune pressure, the evolutionary capacity of this virus could reach far beyond the incorporation of mutations of amino acids comprised within the S-RBD and/ or S-NTD. The only mechanism I could think of being capable to achieve such seemingly ‘incompatible’ effects is, indeed, not a change in the amino acid sequence but a change in the glycosylation pattern. As the spike protein is already glycosylated, potential additional glycosylation should occur in a region that has thus far remained largely exposed and in a way that allows a distinctive impact on anti-NTD Ab binding, depending on whether the virus is free-moving or tethered to tissue-resident DCs.
RBD would likely qualify13 as a candidate for glycosylation since it is less densely glycosylated and presents in dissimilar conformations (i.e., in an ‘open’ [‘up’] or ‘closed [‘down’] state), depending on the context of S expression (i.e., expressed on free virions or on virions attached to DCs or on virus-infected host cells14) and the functional activity of the anti-S Abs (i.e., neutralizing versus non-neutralizing) (https://pubmed.ncbi.nlm.nih.gov/34139176/;https://pubs.acs.org/doi/pdf/10.1021/acscentsci.0c01056; https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7833242/pdf/main.pdf). Until now, however, mutations in dominant variants, including Omicron, have not been reported to affect glycosylation sites (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7253482/). This finding seems to indicate that the glycosylation sites are generally spared by selective pressure, suggesting that they are essential and sufficient for SC-2 infectivity. Inversely, the addition of oligomannose-type glycans could become part of an immune escape strategy in case the virus becomes exposed to additional immune pressure, for example because of enhancing anti-NTD Abs that increasingly compromise its trans infection capacity and, therefore, threaten its transmission. This would be the case in highly vaccinated populations because high prevalence of elevated titers of infection-enhancing anti-NTD Abs will not only cause a milder course of infection but also decrease viral shedding in the vast majority of the population (i.e., in vaccinees; https://www.medrxiv.org/content/10.1101/2022.01.28.22270044v1).
At the bottom of this document, I have attached relevant references from the literature on glycosylation of enveloped viruses, in particular related to SC-2, that may help to understand the biological importance
12 The innate immune system in healthy unvaccinated people is not compromised and its virus elimination strategy does not discriminate between viral variants. Even in the presence of naturally induced anti-S Abs, the immune response in healthy unvaccinated individuals will not discriminate between different SC-2 variants. This is because the innate immune response in unvaccinated, previously exposed individuals is thought to be more protective against the pathogen it got previously exposed to (due to ‘training’) and also because their neutralizing Abs are more likely to match the circulating variant (as compared to the vaccinal Abs) and will be rapidly recalled at high titers. The combination of both arms of the immune system will ensure sterilizing immunity.
13 Glycosylation of the conserved part of NTD itself would not be a suitable alternative as this region is - on purpose- not glycosylated such to enable infection-enhancing Abs to bind to their specific epitopes
14 This already suggests that S expressed on host tissue cells that are transfected with mRNA vaccine could build ‘sterile’ syncytia in the presence of pre-existing anti-S Abs and lead to histopathological alterations in certain organs
Author: G. Vanden Bossche, DVM, PhD March 2022
19
of glycans expressed on spike protein from SC-2 and the role of glycosites and C-type lectins in the immunopathogenic mechanisms explained below.
Is O-glycosylation of RBD feasible and would it provide a logical approach for shielding the conserved enhancing NTD site without compromising enhanced viral infectiousness?
There is extensive evidence that N- and O-glycosylation of viral proteins can not only subvert the innate immune system but also dramatically influence viral infectivity (e.g., by modulating interactions involved in viral attachment to cellular receptors and receptor-mediated entry) and viral virulence. In some cases, though, it seems to be an effect of conformational stability, rather than direct interaction (https://pubmed.ncbi.nlm.nih.gov/26867212/). Glycosylation seems, therefore, an interesting tool for many viruses to overcome selective immune pressure (https://academic.oup.com/glycob/article/28/7/443/4951691; https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7199903/). Glycosylation within a previously exposed domain of RBD, for example, could serve as a protective shield in that glycans can sterically mask the underlying polypeptide epitopes and hence, prevent potentially neutralizing anti-RBD antibodies from recognizing critical binding sites, thereby preventing them from neutralizing SC-2. Viruses take advantage of the host cell machinery for glycosylation and are, therefore, generally decorated with ‘self’-glycans. The latter enable vitally important viral proteins on enveloped viruses to escape the host immune response (https://pubmed.ncbi.nlm.nih.gov/20643940/; https://academic.oup.com/glycob/article/28/7/443/4951691;https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7326345/). By shielding broadly neutralizing epitopes within the S-RBM, more extensive glycosylation on RBD could provide a new variant with an even higher level of infectiousness than Omicron.
It has been reported that the S-RBD in the trimeric S packs tightly with the NTD of a neighboring
chain when the RBD is in the ‘closed’ (i.e., ‘down’) state
(https://pubs.acs.org/doi/pdf/10.1021/acs.jpclett.0c01431;
https://www.science.org/doi/pdf/10.1126/science.abb2507). It is, therefore, tempting to propose
15
that glycosylation be situated on the RBD
.
iii. The high level of inherent conformational flexibility of the RBD region (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7833242/, https://pubs.acs.org/doi/10.1021/acscentsci.0c01056) would render it amenable to a growing number of O-glycosite mutants at the predicted O-glycosylation sites while still preserving its propensity to adopt the open conformation to promote the effectiveness of binding between the RBM and the binding sites on the ACE2 receptor of the host cell.
15 Glycosylation of the conserved part of NTD itself would not be a suitable alternative as this region is - on purpose- not glycosylated such to enable infection-enhancing Abs to bind to their specific epitopes
Author: G. Vanden Bossche, DVM, PhD March 2022
20
Why would O-glycosylation be more likely than N-glycosylation?
SC-2 has already probed insertion of O-glycosylation, namely next to its fusion site, most likely as a strategy to counter immunological pressure in some intermediate host (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7645279/). Dense O-glycosylation of viral proteins has already been described to provide ‘bulk’ shielding from select immunodominant epitopes (https://pubmed.ncbi.nlm.nih.gov/22114560/).
In contrast to N-glycosylation, O-glycosylation is much more versatile as O-linked glycans could be
16 anchored on several amino acids (e.g., serine, threonine, tyrosine) within the RBD .
(https://www.biorxiv.org/content/10.1101/2020.07.05.187344v1.full.pdf). In addition, 2 predictive O-linked glycosylation sites located at the N-terminal edge of the RBD have already been identified (see also further below; https://pubmed.ncbi.nlm.nih.gov/32366695/).
It has been reported for other enveloped glycosylated viruses (i.e., Alpha Herpesviruses) that sequence homology is an important determinant for O-glycosylation in closely related viruses (Herpes simplex type 1 and 2) in that homologous glycosites are mainly situated on highly homologous peptide sequences (https://pubmed.ncbi.nlm.nih.gov/27129252/). Hence, in order for O-glycosylation to successfully and consistently overcome selective immune pressure during a pandemic of variants, it likely suffices when it occurs in a region of the RBD that is largely conserved. This would ensure a consistent stabilization effect of the glycan moieties on the conformation of the RBD.
Based on all the above, it is fair to conclude that a single or very few mutations enabling the incorporation of one or more additional O-glycosites could be an effective strategy to shield epitopes against both anti-RBD and anti-NTD Abs.
Could O-glycosite mutants decouple enhanced viral infectiousness from diminished pathogenicity in vaccinees by enabling trans fusion?
This statement already suggests that O-glycosylation can overcome remaining immune defense strategies that are protecting the vaccinated host from severe disease while still ensuring a high level of viral infectiousness.
A highly vaccinated population that is repeatedly exposed to a highly infectious SC-2 variant that is largely resistant to neutralizing Abs will exert high immune pressure on viral trans infectiousness (via the enhancing anti-NTD Abs), which is conditioning systemic viral disease. This is currently suppressing the capacity of the virus to become more virulent. Because of the high immune pressure exerted by the enhancing anti-NTD Abs of vaccinees, it is likely that a phenotype will be selected that can abolish Ab-
16 The RBD of SC-2 comprises several amino acids that are known to be susceptible to O-glycosylation. Some of them have already been identified as a predicted O-glycosylation sites. Natural selection may provide for O- glycosylation of a predicted O-glycosylation site or for an amino acid context promoting O-glycosylation of one or more eligible amino acids at a well-defined site occupancy
Author: G. Vanden Bossche, DVM, PhD March 2022
21
mediated hindrance of trans infection between virus-loaded, migrating DCs and uninfected target cells in the LRT or distant organs and, therefore, achieve a higher level of virulence/ pathogenicity. Any viral variant that is capable of restoring the capacity of S-NTD to induce fusogenic rearrangement of S without jeopardizing the enhanced infectiousness of the virus would qualify. This reasoning is consistent with observations made in avian influenza epidemics in chicken, where high infectiousness and rapid transmission in highly dense chicken populations selects for a more fusogenic hemagglutinin (HA) protein (which serves a function similar to that of the coronavirus spike protein). Variants that incorporate a polybasic cleavage site (already present in SC-2 spike protein!) in their hemagglutinin (HA) protein can enhance fusogenic rearrangement of HA and, therefore, strengthen the capacity of the virus to infect distant target cells in trans. The selection of a more fusogenic HA variant has enabled avian influenza viruses to evolve from low-pathogenicity into highly pathogenic variants (https://www.nature.com/articles/s41591-020-0820-9.pdf).
In view of some preliminary evidence that anti-NTD Abs could prevent progression to severe disease (https://www.nature.com/articles/s41586-021-03925-1.pdf), it is tempting to hypothesize that O- glycosylation of the RBD may enable the virus to counter the effect of infection-enhancing anti-NTD Abs and thereby block inhibition of viral trans infection in distant organs including, but not exclusively restricted to, the LRT. As will be explained below, this seems totally plausible from a biophysical viewpoint.
It is, therefore, tempting to predict that the upcoming predominantly circulating variants will be endowed with a more densely O-glycosylated RBD and that this feature will confer resistance to both, potentially neutralizing and infection-enhancing anti-S Abs in vaccinees, thereby providing this new ‘family’ of ‘super variants’ (for the purpose of this report referred to as ‘Newco’ variants) with the capacity to use their enhanced infectiousness (i.e., ADEI) for potentiating their pathogenic capacity/ virulence (i.e., leading to ADED) while allowing for rapid replacement of the Omicron family and an explosive spread across the globe.
The impact of O-glycosylation on the immune pathogenesis of SC-2 in highly vaccinated populations exposed to a largely vaccine-resistant SC-2 variant (i.e., Omicron) is summarized in fig. 4.
How could O-linked glycosylation promote viral virulence in vaccinees?
As binding of the enhancing site of the NTD by specific infection-enhancing anti-NTD Abs is thought to hamper trans infection by close state-constrained virions tethered to migratory DCs, it would be important for the virus to use a glycosylation strategy that dampens binding of the infection-enhancing anti-NTD Abs to their corresponding epitopes such as to restore its ‘trans infectiousness’. However, glycosite mutations should not affect the conformation of the enhancing site itself as this would prevent anti-NTD Abs from inducing the open RBD conformation on free virions, which is key to inducing enhanced recognition of ACE2 receptors by RBD and, therefore, critical to maintain a high level of infectiousness.
This challenge could be solved by expansion of glycosylation on another conserved part of S that has the capacity to shield the specific infection-enhancing epitopes on NTD without changing the conformation of NTD. It has been reported that the S-RBD packs tightly with the S-NTD of a neighboring chain when
Author: G. Vanden Bossche, DVM, PhD March 2022
22
the RBD domains are held in the closed position (as is the case when the virus is adsorbed on DCs) [https://pubs.acs.org/doi/pdf/10.1021/acs.jpclett.0c01431]. It is, therefore, tempting to propose that additional glycosylation should occur on the RBD. Because of the closed position of RBD when the virus is tethered to DCs, site-specific glycosylation on the RBD could shield the specific conserved infection- enhancing domain within NTD and thereby prevent infection-enhancing Abs from binding and inducing conformational changes, which, as explained above, would hamper fusogenic rearrangement of S that is normally facilitated by the NTD’s ganglioside-binding domain (see fig. 5; left panel). This could prevent inhibition of trans infection from migratory DCs to distant target tissue cells and, therefore, allow for systemic dissemination of the infection while still also allowing the infection-enhancing Abs to bind to free virions to mediate ADEI (see section below: ‘Could O-linked glycosylation also allow for resistance to the C-19 vaccines?’).
However, to cause as little as possible steric hindrance to the interaction between the RBM and ACE2, glycosylation should take place at a distance as far as possible from the RBM. It is interesting to note that 2 predictive O-linked glycosylation sites located at the N-terminal edge of the RBD have been reported, one at threonine 323 and another at serine 325. The function of these predicted O-linked glycans has not yet been elucidated. The O-linked glycosylation could only be detected at trace levels, suggesting that O-linked glycosylation of this region is minimal when the structure is native-like (https://pubmed.ncbi.nlm.nih.gov/32366695/). It is tempting to speculate that - in conjunction with the 2 neighboring N-glycan chains (N331 and N343) - the O-linked glycosylation sites provide SC-2 with ample flexibility to grow its pathogenic capacity in case reduced shedding and insufficient virulence (i.e., fewer cases of systemic disease) would be threatening the life cycle of the virus (i.e., as a result of immune pressure exerted by the infection-enhancing anti-NTD Abs). This capacity could readily be expanded by an increase in site occupancy of the O-linked glycans. In case of a strong impediment of ‘trans infection’, the extent of O-glycosylation at the predictive sites could progressively increase in response to natural selection based on a competitive fitness advantage to be gained in the context of immune pressure from enhancing anti-NTD Abs. O-glycosylation at the N-terminal end of the RBD is likely to shield the binding site for these enhancing Abs when RBD is in the closed state17 and thus, in close contact with the region comprising the enhancing epitopes. This is to say that an important addition of glycosites to the RBD could affect the conformation of the NTD. Changes in the N- glycosylation of NTD, for example, have been reported to impact the conformational dynamics of the RBD (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7523240/pdf/oc0c01056.pdf). Likewise, it is reasonable to expect that a more densely glycosylated RBD will induce conformational changes in the NTD when RBD is stabilized in the closed conformation via lectin-mediated binding of the virus to DCs. As the NTD is known to modulate the conformational dynamics of the RBD via N-linked glycosite chains18(https://pubs.acs.org/doi/pdf/10.1021/acs.jpclett.0c01431; https://www.science.org/doi/pdf/10.1126/science.abb2507), a structural change of the NTD would be at risk of preventing it from triggering the open conformation of RBD and thereby reducing the
17 In the ‘closed’ position, the O-glycosylated chains are likely to contribute to the interaction of the N-glycan patch with DC surface-expressed C-type lectins and would thereby contribute to stabilizing the ‘closed’ position
18 NTD-associated glycans (i.e., N165 and N234), for example, have been reported to modulate the conformational plasticity of the RBD (https://pubs.acs.org/doi/pdf/10.1021/acscentsci.0c01056)
Author: G. Vanden Bossche, DVM, PhD March 2022
23
opportunity for the contact surface of the RBD region (i.e., RBM) to interact with the ACE2 receptor. The higher the density of the glycosylation, the higher the risk that the glycan shield would no longer be optimally paired with the conformation of NTD that is required to mediate optimal fusogenic capacity. As structural glycosylation-induced rearrangement of NTD would be at risk of hampering trans infection of the virus tethered to DCs, it would make sense for the virus to naturally select amino acid mutations within the variable region of NTD to compensate for the lack of capacity of NTD to induce fusogenic rearrangement of S and thus, enable trans infection. This should be perfectly feasible as it has been reported that the conformational state of the RBD is largely dependent on the regions around the epitopes that are recognized by the infection-enhancing Abs (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8142859/pdf/main.pdf). It is, therefore, fair to conclude that the immune pressure exerted on the single conserved enhancing site within NTD would ultimately translate into steric pressure on the variable antigenic sites within NTD that are situated around the enhancing site. This is likely to drive selective incorporation of a certain number of amino acid mutations within these highly variable domains of NTD such as to prevent the growing glycosylation density of the O-linked sites on the RBD from compromising the capacity of NTD to trigger the fusogenic rearrangement of S upon contact of DC-loaded virions with distant tissue-resident target cells.
In summary (see also fig. 5; left panel):
- Ab-mediated immune pressure on the conserved enhancing site within S-NTD drives natural selection of enhanced O-glycosylation on the S-RBD
- Enhanced O-glycosylation of the S-RBD drives natural selection of amino acid mutations within the variable regions of S-NTD
- Ab-mediated immune pressure exerted on the epitopes comprised within the conserved enhancing NTD site translates into steric pressure on the variable epitopes that are situated around the conserved epitopes recognized by the infection-enhancing Abs
- Selective amino acid mutations will enable the virus to overcome population-level immune pressure exerted on its capacity to trans infect distant host tissue cells (i.e., to cause systemic disease)
Because the evolutionary variability of NTD is higher than that of the rest of S (https://www.frontiersin.org/articles/10.3389/fmicb.2020.02112/full), it can be expected that there is still plenty of capacity for the epitopes around the conserved infection-enhancing epitopes to evolve by incorporating amino acid mutations that enable to counter the negative impact of the O-glycosylation- mediated conformational changes in NTD on the latter’s capacity to trigger fusogenic rearrangement of S (i.e., to restore the ‘trans infectiousness’ of the virus at the level of the LRT and possibly other distant organs).
Based on all the above, it is fair to conclude that ADEI in the URT as a result of poor virus neutralization capacity would dramatically increase the amount of infectious SC-2 virions that are captured and contained by DCs resident in the mucosal tissue at the portal of viral entry and would, therefore, dramatically expand the reservoir the infectious virus can spill over from to different distant organs to trigger ADED in the LRT once the trans infection barrier has been lifted. It is tempting to speculate that O-glycosylation of the RBD is capable of lifting this barrier. The additional incorporation of one or more amino acid mutations within a (highly) variable part of NTD that is adjacent to the enhancing domain is
Author: G. Vanden Bossche, DVM, PhD March 2022
24
thought to serve as an elegant and effective strategy for allowing O-glycosylated Newco variants to restore optimal trans infectiousness and allow for ADEI-mediated ADED.
It is certainly conceivable that a higher O-glycosylation density on the RBD could also enhance trans infection (i.e., by joining the cluster of N-glycans recruited by DC surface-expressed C-type lectins and thus strengthening viral attachment to the URT-resident DCs) and even trans fusion between virus- infected and not infected cells at distant target organs (i.e., by promoting the interaction between oligomannoyslated glycans on S expressed at the surface of SC-2 infected cells and glycan-binding determinants on uninfected neighboring cells). It is, therefore, reasonable to assume that site-specific O-glycosylation on RBD would not only restore viral trans infectiousness (i.e., by impeding binding of the infection-enhancing Abs) and, therefore, its trans fusion capacity, but that it would even strengthen viral trans fusion and hence, enhance the likelihood of causing systemic C-19 disease. This will only augment the severity of ADEI-mediated ADED.
It is, therefore, fair to posit that more abundant O-linked glycosylation could make SC-2 highly virulent in vaccinees and, therefore, make vaccinees highly susceptible to severe systemic disease.
Could O-linked glycosylation also allow for resistance to the C-19 vaccines and, therefore, provide for a high level of viral infectiousness in vaccinees?
‘Yes’, it would even allow Newco variants to achieve full resistance to the C-19 vaccines and further increase ADEI in vaccinees.
Importantly, O-glycosylation of the S-RBD would not prevent the S-RBM from interacting with the ACE2 receptor when the RBD is in the open conformation as a result of enhancing Abs binding to the conserved site of S-NTD. This would apply to SC-2 virions that are free-moving in the URT (i.e., not restrained by DCs). It follows that O-glycosylation of S-RBD is unlikely to disturb Ab-dependent enhancement of viral entry into epithelial cells of the URT (see fig. 5; right panel). It follows that the RBM of free Newco virions will now bind with high affinity to the ACE2 receptor on target cells in the URT. This would largely prevent potent, broadly neutralizing Abs from blocking the binding of their RBM to the ACE2 receptor (https://www.nature.com/articles/s41586-021-04386-2).
Consequently, it is fair to conclude that while enhanced O-glycosylation at the N-terminal end of the RBD did not result from selective immune pressure on broadly neutralizing epitopes within the RBM (as the RBM is only poorly immunogenic anyway;https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7833242/), it nevertheless contributes to further strengthening ADEI19 occurring at the URT.
On the other hand, O-glycosylation would also facilitate resistance to potentially neutralizing Abs that are directed at variable epitopes on the S-RBD. Whereas O-glycosites inserted at the N-terminal end of RBD would initially substitute for the amino acid mutations that are shielded by the inserted glycans,
19 A further decrease in neutralization capacity entails more binding of the enhancing NTD site by non-neutralizing, high-affinity anti-NTD Abs and, therefore, strengthens ADEI
Author: G. Vanden Bossche, DVM, PhD March 2022
25
and which were initially incorporated by Omicron to confer resistance to these Abs, they could
ultimately preclude immune recognition of the variable RBD region all together. This would dramatically
relieve the constraints on natural selection of these epitopes for new, O-glycosylated variants. Shielding
of the variable RBD epitopes by O-linked glycosites would not depend on whether the RBD is in the open
or closed state as it has been documented that glycans bound to the RBD region itself equally shield/
protect the region that does not directly interact with ACE2 in both the ‘closed’ and ‘open’ position
(https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7523240/). It is known that the insertion of an
additional glycan chain on S in SC-2 can efficiently mask underlying polypeptide epitopes in that in vitro
escape of SC-2 from highly neutralizing COVID-19 convalescent plasma has been shown to include the
insertion of a new glycan sequon in the N-terminal domain of S as a mechanism to provide complete
resistance to neutralization (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7781313/). Taken
together, it is fair to conclude that O-linked glycosylation of the RBD has the capacity to ensure full viral
resistance to not only the existing C-19 vaccines but even to any future ‘update’ of an S-based C-19
20 vaccine .
The overall effect of O-glycosylation of the S-RBD on the immune pathogenesis of potential Newco variants has been summarized in fig. 6.
In summary, the O-glycosylated Newco variants would be ideally equipped for countering selective immune pressure exerted by the vaccinated population on the conserved ‘enhancing’ domain of NTD while also provided with the capacity to further strengthen ADEI, and thus cause ADED in vaccinees as a result of their enhanced resistance to vaccinal Abs induced by S-based C-19 vaccines.
What would be the consequences of site-specific O-glycosylation on the phenotypic characteristics of the virus?
From the viewpoint of viral evolution, there should always be a strong selective pressure favoring the protection of a region that is crucial for the viral life cycle. By expanding glycosylation of the N-terminal end of its RBD, SC-2 could protect the S-NTD from anti-NTD Abs that ‘neutralize’ trans infection (by DC- bound virions) while also protecting the S-RBD from anti-RBD Abs that ‘neutralize’ infection (by free virions). This would result in an enhanced level of both viral virulence and viral infectiousness in vaccinees and thereby rise their risk for contracting ADED.
I anticipate that natural selection of enhanced site occupancy of only a few predicted O-glycosylation sites at the N-terminal end of S-RBD would already suffice for virions tethered to DCs to overcome high immune pressure exerted by the vaccine-induced enhancing Abs on S-NTD while enabling the same Abs
20 Updated vaccines would incorporate the genetic code (i.e., in the case of genetically engineered vaccines) or sequence (i.e., in case of protein-based or inactivated vaccines) of the variant S-derived polypeptide, which, however, would be shielded in the circulating Newco. Vaccines using conjugated glycans to target O- or N- glycosites would obviously be at risk of inducing auto-reactivity. It cannot be ruled out that abnormal (i.e., insufficient) activation of DCs by S-based genetic vaccines is already inducing such auto-immune responses because of strong antigen-presentation of SC-2-derived glycopeptides.
Author: G. Vanden Bossche, DVM, PhD March 2022
26
to provide free virions with an even higher level of infectiousness in vaccinees (as compared to the level of infectiousness achieved by Omicron).
In conclusion, it seems perfectly feasible for O-glycosylation of the RBD to not only fulfill the requirements for enhanced viral entry via a higher level of binding of infection-enhancing Abs to a conserved nonglycosylated site on the S-NTD but also for enhanced trans infection via shielding against the very same Abs as provided by its glycosylated counterpart (i.e., the RBD). This directly results from a higher level of resistance of the O-glycosylated S to potentially neutralizing Abs induced by the vaccine combined with a higher susceptibility of O-glycosylated S to fusogenic rearrangement. Vaccinees exposed to Newco variants would, therefore, be at an even higher risk of ADEI and, therefore, prone to contract ADED.
In other words, O-glycosylation at the N-terminal of the RBD is likely to further enhance ACE2- dependent, anti-NTD Ab-mediated virus-cell fusion, thereby leading to an even more pronounced ADEI effect, which in turn would trigger ACE2-independent anti-NTD Ab-mediated enhancement of cell-cell fusion and thereby lead to ADED. This is completely in line with the overwhelming evidence from the literature that viral glycosylation has the capacity to modulate both viral infectiousness and viral virulence and enable resistance to Abs that exert immune pressure but in ways that don’t prevent viral infection or block viral transmission (https://pubmed.ncbi.nlm.nih.gov/29579213/; https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7781313/).
How would the O-glycosylated Newcos evolve in a highly vaccinated population and what would be their impact on individual and public health?
From the evolutionary dynamics discussed above, it becomes already apparent that increased population-level immune pressure on the conserved enhancing NTD site will result in natural selection of more abundantly glycosylated and, therefore, more virulent and more infectious variants. Since the O-glycosite mutations, as well as the required accompanying amino acid mutations within the variable domains of NTD, would have to keep up with the steadily increasing immune pressure exerted by the vaccinated population on the conserved infection-enhancing NTD site, both virulence and infectiousness of naturally selected variants would steadily rise too. More infectious and more virulent Newco variants that have a competitive fitness advantage over Omicron would successively be replaced by other Newco variants with an even higher level of infectiousness and virulence and, therefore, with an even higher fitness advantage in the context of a highly vaccinated population. With each more infectious and more virulent selected Newco the number of infections causing severe disease and death would gradually but rapidly increase whereas the corresponding fitness intervals would become shorter and shorter (see fig. 7). In highly vaccinated countries waves would rapidly add up one on top of the other to finally build a massive wave of severe morbidity and death that could last for as long as viral infectivity rates and, therefore, the prevalence of elevated ‘infection-enhancing’ Ab titers rises.
In a highly vaccinated population that is continuously exposed to SC-2 variants that continuously improve on escaping from potentially neutralizing Abs, enhanced virulence and enhanced infectiousness will inevitably be linked to one another. This would already suggest that with rising population-level
Author: G. Vanden Bossche, DVM, PhD March 2022
27
immune pressure on viral trans infectiousness (i.e., on virulence) cases of C-19 disease would not only rapidly grow in number but also in severity. It also indicates that this dramatic evolution of the virus will only stop if the population-level immune pressure from the infection-enhancing Abs drops. If we leave it up to the virus, this can only happen if the population shrinks as a result of enhanced viral virulence.
From a viewpoint of individual health, it seems obvious that the susceptibility of vaccinees to contract ADED (mediated by ADEI) would augment with growing expansion in prevalence of Newcos.
How long will it take for more pathogenic SC-2 variants to become dominant?
As the adequate combination of O-glycosite mutations on RBD and amino acid mutations within NTD may take time to select, it is reasonable to expect that it will take ‘some more time’ for the first Newcos to emerge. However, there are several different reasons that make me believe that the virus will now rapidly evolve into more virulent and more infectious variants. In other words, I expect the lag time for a first more virulent variant to cross the valley of fitness and begin to replace Omicron to be rather short (i.e., within 2 months following this date of writing).
Why?
First, there seems to be a lot of room for additional O-linked glycosylation on SC-2’s spike protein (even without involving the bulk of the RBD). In addition, it is likely that denser O-glycosylation patterns on the RBD would initially only require very few amino acid changes in the highly variable NTD domain to compensate for the steric pressure placed by early RBD glycosylation on the trans infection capacity of the virus.
But even the incorporation of a growing number of adequate amino acid mutations enabling RBD glycosylation doesn’t seem very problematic as mutations could now accumulate quite rapidly because of more frequent recombination events and inter-species as well as intraspecies transmission. Since cross-species transmissibility seems to be determined by conservation of the RBM (i.e., a motif comprising a limited number of amino acids that are essential for efficient binding of SC-2 to the ACE2 receptor), SC-2 (including Omicron) can infect several different animal species (https://bmcresnotes.biomedcentral.com/track/pdf/10.1186/s13104-020-05242-8.pdf). This already suggests that reverse zoonosis events are now occurring more frequently (https://www.sciencedirect.com/science/article/pii/S0168170221001805). Omicron is, therefore, highly likely to establish new and even larger animal reservoirs of SC-2. But especially also the vaccinated human population is now increasingly serving as an important reservoir for the virus as vaccinal Abs mediate enhanced infection rates in vaccinees (https://www.medrxiv.org/content/10.1101/2022.01.28.22270044v1). In other words, there is plenty of opportunity for the virus to replicate and transmit and, therefore, to mutate and recombine. This provides the virus with a growing arsenal reservoir of mutations to select from.
Furthermore, the high level of conformational plasticity of both the NTD and the RBD (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7962585/;
Author: G. Vanden Bossche, DVM, PhD March 2022
28
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7953435/; https://pubs.acs.org/doi/pdf/10.1021/acscentsci.0c01056) likely allows for several distinct combinations of O-glycosite mutations in the RBD and amino acid mutations in the NTD that all comply with natural selection for enhanced virulence combined with higher infectiousness.
In addition, the selection criteria for viable mutations in the NTD of potential Newcos are not very stringent as it is likely that several distinct amino acid mutations, or a combination thereof, will manage to compensate for the conformational change in NTD that is triggered by O-glycosylation of the RBD when the latter is stabilized in the closed position.
Last but not least, the selection pressure on RBD for conserving the critical amino acid mutations selected by Omicron would likely wane with additional O-glycosylation of RBD and could be fully relieved as this part of S would no longer be crucial for the life cycle of Newco variants. This is to say that Newco variants will likely be featured by a substantial level of antigenic variability of both S-NTD and S- RBD.
Based on the above considerations, it seems fair to predict that natural selection of adequate Newco variants will not only occur rapidly but that adequate selections in highly vaccinated populations across the globe could also occur completely independently. Regardless of the variability in their antigenic constellation (which could be quite different depending on their geographical site of emergence), selected Newcos would spread equally well in all highly vaccinated populations currently exposed to Omicron. This is because their infectiousness for these populations would not be impacted by their enhanced antigenic variation in the non-conserved RBD and NTD region (cfr. above). It is, indeed, obvious that this variability would neither affect binding of the infection-enhancing anti-NTD Abs to the conserved antigenic site of NTD nor binding of the conserved RBM to ACE2.
In the meantime, several new variants could emerge due to active recombination or reassortment events that result from co-infection and/or further evolution in animal species. Although new viral variants are continuously identified, some of which share characteristics of other very distinct variants (e.g., Deltacron, Combicron,...), none of them will have a chance to outcompete Omicron unless they comply with the selection criteria explained above.
In conclusion, I predict that within the context of the currently prevailing population-level immune pressure exerted by infection-enhancing anti-NTD Abs, the likelihood that more and more immune escape variants will spread faster and faster in highly vaccinated populations and manifest a more and more infectious and increasingly virulent behavior in vaccinees is now dramatically increasing.
In healthy non-vaccinated individuals, O-glycosylated Newcos will only cause asymptomatic to mild disease
Several enveloped viruses (including CoV) are decorated with carbohydrates synthesized by host cells and capped by ‘self’ sugars (e.g., sialic acid) which are sensed by sialic-acid-binding immunoglobulin-like lectins (Siglecs) expressed on the surface of innate immune cells, which use this signaling to produce immune inflammatory mediators (e.g., cytokines). The glycans exposed on S protein and other viral
glycoproteins have been synthesized by the glycosylation machinery of the host and are, therefore, self- 29
Author: G. Vanden Bossche, DVM, PhD March 2022
glycans. These self-derived viral glycans are used by the virus as an elegant strategy to mask ‘nonself’ viral peptides and hence, shield the host immune response. It is important to note that the S protein contains substantial populations of ‘altered’ or ‘self-like’ glycosylation patterns in that the processing of S glycans can greatly differ from that of host glycoproteins as, for example, exemplified by the presence of several S-associated glycosylation sites containing substantial oligomannose-type glycans (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7199903/). Likewise, ‘self-like’ glycan patterns can be recognized by BCRs on B1a-derived innate effector cells. It is, therefore, not surprising that SC-2 and other enveloped viruses that carry glycosylated proteins on their surface can be recognized by innate B1a-derived cells (https://www.nature.com/articles/s41435-020-0105-9.pdf ). Activation of these cells is thought to stimulate their production of polyreactive natural (I prefer the term: ‘innate’) antibodies of relatively low affinity that are primarily of the polymeric IgM isotype. They could thereby facilitate NK cell-mediated killing of virus-infected cells that display self-like glycan patterns on their surface at an early stage of infection and at the very portal of entry (i.e., the URT). In line with the epigenetic mechanism of innate immune adaptation to changes in environmental exposure and the instructive role of BCR signaling in B1a cell development (https://www.nature.com/articles/s41577-020-0285-6.pdf; https://www.jimmunol.org/content/204/1_Supplement/241.3;https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5943138/pdf/nihms934113.pdf), it is highly plausible that following their activation as a result of viral exposure, B1a innate immune cells can be instructed to reprogram and improve their functional activity (‘training’) such as to recognize alterations in self-like glycosylation patterns that are caused by mutations of O-glycosylated sites. As the additional O- glycosites would equally be synthesized by the glycosylation apparatus of the host, it is reasonable to assume that the efficiency of recognition of the overall glycan pattern exposed on the surface of S will not suffer from incorporation of additional O-glycosite mutations. On the contrary, I postulate that the above-described alteration to the self-derived glycosylation pattern on S will only enhance activation and long-term functional reprogramming of self-recognizing innate immune cells to provide relevant innate polyreactive IgMs with enhanced affinity for the new O-glycosylated variants. This would not only improve the protective effect of these Abs against the virus but also ameliorate their capacity to compete with potentially acquired infection-enhancing S-specific Abs. Innate immune training is, therefore, thought to render the immune response to subsequent CoV infections more effective. This postulate seems to be confirmed by recent data published by UK Health Security Agency (UKHSA), showing that vaccine effectiveness has now become strongly negative across all age groups (https://www.gov.uk/government/publications/covid-19-vaccine-weekly-surveillance-reports). It is interesting to note that at least one team of researchers seems to appreciate that innate, polyreactive Abs may compete with anti-NTD Abs for binding to the infection-enhancing site on NTD. They literally state:
“It is noteworthy that uninfected individuals possess antibodies that recognize the infectivity-enhancing site on the NTD, albeit at quite low frequency. Because the epitopes of enhancing antibodies contain charged residues, it is possible that binding to the NTD is mediated by polyreactive antibodies. However, serum antibodies against the infectivity-enhancing site did not bind to the RBD transfectants, suggesting that binding was specific to the infectivity-enhancing site”(https://www.sciencedirect.com/science/article/pii/S0092867421006620). These authors also established that non-infected individuals could recognize both the wild-type and mutant NTD. As
Author: G. Vanden Bossche, DVM, PhD March 2022
30
infection-enhancing Abs are highly specific, the recognition of the infection-enhancing epitopes by uninfected individuals is to be considered non-specific and, therefore, their Abs are not to be considered infection-enhancing. Because Ab epitopes on the enhancing site of NTD are conserved among SC-2 variants but not among CoVs in general (https://www.sciencedirect.com/science/article/pii/S0092867421006620), enhancement of infection would not occur with facilitating anti-NTD Abs that have been induced as a result of previous CoV infection. Innate, polyreactive Abs, however, are thought to react with a large spectrum of glycosylated enveloped viruses and certainly with different CoVs. This seems to be confirmed by the observation that anti-NTD Abs in uninfected individuals were able to react with both wild-type and mutant NTD (https://www.sciencedirect.com/science/article/pii/S0092867421006620).
Furthermore, it can even be expected that in the absence of infection-enhancing anti-NTD Abs (i.e., in non-vaccinated individuals), more abundant O-linked glycosites grafted on sequons at the N-terminal end of the RBD would no longer adequately synergize with the amino acid mutations inserted in the variable NTD region to prevent O-glycosylation from hindering trans infection. Lack of infection- enhancing anti-NTD Abs in the non-vaccinated would, therefore, not only diminish infectiousness of free-moving SC-2 virions (including Newcos) in the URT but also debilitate ‘trans infectiousness’ of SC-2 virions (including Newcos) attached to migrating DCs or pulmonary epithelial cells. It is tempting to speculate that even those whose innate immune system is weakened and/ or did not sufficiently benefit from epigenetic ‘training’ of their innate IgM producing B cells would benefit from the reduced viral infectiousness and virulence, provided they are not vaccinated. Whereas Newco infections could be fully asymptomatic in the vast majority of the non-vaccinated individuals, Abs induced in those who would still be susceptible to developing some form of disease could possibly prime broadly cross-protective
21 neutralizing Abs as a result of enhanced immunogenicity .
In conclusion: For the vast majority of the unvaccinated, the price to pay for training of their innate immune effector capacity will not exceed mild to moderate upper respiratory symptoms. For this part of the population, new, more densely O-glycosylated variants could even be considered improved editions of a ‘live attenuated vaccine’ due to their steadily increasing intrinsic attenuation (because of the growing O-glycosylation). Their enhanced attenuation would, indeed, only come to bear in non- vaccinated individuals as the protective innate immune capacity of the unvaccinated will not be compromised by vaccine-mediated immune priming. This already suggests that C-19 vaccine effectiveness, which already turned negative, will become even more negative in all age groups . It
21 Immunogenicity would likely be conferred by the ‘non-compensated’ conformational change in the RBM that would occur when virions attach to migrating DCs
22 Initially, vaccine effectiveness was only found to be negative in older age groups (> 18y), probably because their innate Ab were better ‘trained’ to recognize self-like glycan patterns on enveloped viruses compared to those of young children, whose innate Abs have less affinity and would, therefore, be readily outcompeted by infection- enhancing vaccinal Abs known to provide better protection against severe disease. However, as shown by more recent data from UKHSA, unvaccinated children can rapidly catch up on innate immune training as they become more and more exposed to the virus. Re-exposure to evolving viral variants is thought to trigger long-term functional reprogramming of innate immune cells as a result of their activation and thereby enable enhanced responses to subsequent infections https://www.nature.com/articles/s41577-020-0285-6
22
Author: G. Vanden Bossche, DVM, PhD March 2022
31
further strongly suggests that will be highly unlikely for Newcos to cause ADEI in the non-vaccinated. Consequently, it would be highly unlikely that non-vaccinated people contract ADED.
Why are C-19 vaccinated people no longer able to rely on relevant innate immune cells when circulating variants become resistant to the neutralizing capacity of the vaccinal Abs?
Neutralizing anti-S Abs have strong affinity for SC-2 as they are primarily directed at immunodominant epitopes within the S-RBD. Because of their high affinity, these Abs can easily outcompete innate polyreactive IgM Abs that recognize self-like glycans on the surface of CoV. In case there is sufficient match between the immunodominant RBD epitopes and the vaccine-induced Abs, this does not pose a problem to controlling viral infection and spread. In the absence, however, of sufficient virus- neutralizing capacity of vaccine-induced Abs (due to resistance of the virus to potentially neutralizing anti-S Abs), these innate polyreactive IgM Abs can still be outcompeted by non-neutralizing, infection- enhancing anti-NTD Abs that are equally elicited by all S-based C-19 vaccines (see fig. 3). As the enhancing NTD site is relatively conserved (i.e., shared among all different SC-2 variants), the enhancing Abs will be recalled upon re-exposure with new immune escape variants and bind with disproportionally high affinity to S if the neutralizing capacity of the vaccinal Abs towards the circulating variant is low. Unless the functional capacity of the relevant innate immune cells has been sufficiently trained before vaccination such as to produce relevant polyreactive IgM of higher affinity, the infectious and pathogenic behavior of SC-2 in vaccinees will be largely determined by their vaccine-induced enhancing Abs, especially as those will continuously be boosted by virtue of the dominant circulation of the vaccine-resistant variant.
Lessons from Nature
Many CoVs and vertebrates have evolved together a sound balance between host and viral interests, resulting in an equilibrium that is long-term but not necessarily forever stable. CoVs have developed evolutionarily stable strategies that permit homeostasis such as to enable the virus to establish a persistent relationship with human hosts. Mass vaccination has profoundly disturbed the capacity of the host to control transmission and spread of the virus by shifting the host’s most powerful (i.e., conferring sterilizing immunity) and natural line of immune defense against CoV towards a vaccine-induced immune response that is not sterilizing and, therefore, cannot generate herd immunity and thus, cannot control the virus. This prevents virus-host interactions from establishing a well-balanced viral host ecosystem that ensures viral persistence in a healthy population. In case of a pandemic of an acute self- limiting infection, herd immunity is an absolute prerequisite for ending the pandemic phase and driving the virus into endemicity. However, this state of sound equilibrium between the host and the virus cannot be achieved for as long as the host population massively launches non-sterilizing immune attacks to fight the virus. In the absence of vaccines inducing sterilizing immunity, the only immune strategy a population can use to effectively control the virus and to prevent it from evolving into dominant immune escape variants is to ensure people make best use of their innate immune defense (via ‘training’ of a healthy immune system!) to sterilize the bulk of viral load.
Author: G. Vanden Bossche, DVM, PhD March 2022
32
In people whose innate immunity is struggling to abrogate CoV infection and, therefore, requires assistance from short-lived, MHC-unrestricted cytotoxic CD8+ T cells23 to clear the virus, S-specific Abs will be induced and rapidly recalled upon the next exposure to assist the innate immune system in providing sterilizing immunity. In case of a natural pandemic, these Abs will, indeed, have sufficient neutralizing capacity to deal with the next variant, unless it is very different from the previous one (e.g., in case of antigenic ‘shift’). Consequently, sterilizing immunity against CoVs can be conferred by (trained) natural immune effector cells (i.e., innate B1a cells producing polyreactive IgM, potentially joined by recalled antigen-specific Abs produced by B memory cells).
Neutralizing S-specific Abs together with ‘training’ of the innate immune system, as a direct consequence of its exposure to the evolving virus, will strengthen the overall sterilizing capacity of the host’s immune defense. When this capacity has grown large enough at a population level, the pandemic will transition into an endemic stage, which is characterized by a very low viral transmission rate. Once endemic, the virus will remain under control for as long as the infectious pressure (generated because of asymptomatic intra- or interspecies transmission) doesn’t grow large enough to break through the immune defense of a (vulnerable) part of the population. When this happens - even if only affecting a small part of the population - an outbreak may be initiated on a background of viral endemicity.
Since herd immunity requires strong innate immunity as a foundation and since the functional capacity of relevant innate IgMs is likely compromised in vaccinees (even if the vaccines ‘do no longer work’), chances are slim for a highly vaccinated population to achieve a level of sterilizing immunity that cuts the chain of transmission. It follows that as long the population’s first line of innate immune defense against CoV is suppressed, it will fail to sufficiently tame the virus to drive it into endemicity and prevent it from evolving more dangerous variants, even if, for now, it predominantly causes mild symptoms. It is, therefore, not irrational to postulate that natural selection based on fitness and immune pressure will lead to dominant propagation of SC-2 variants that continue to fuel the pandemic for as long as a population predominantly consists of people whose innate immune defense against CoVs (including all SC-2 variants) is too weak or suppressed. It inevitably means that the pandemic will continue for as long as the majority of the population continues to boost their non-neutralizing, infection-enhancing vaccinal Abs (e.g., as a result of highly infectious variants circulating). This implies that to ‘actively’ end the pandemic, the population would need to either prevent their vaccinal Abs from being recalled all the time or to beef up its pool of unvaccinated people such as to raise their share to a percentage that in the
24
past has proven high enough to successfully control similar natural pandemics . If no drastic large-scale
antiviral chemoprophylaxis program is started, herd immunity could only naturally occur in the following ways:
1. A massive baby boom, which, however, is not a realistic solution as it would come too late
2. Massive immigration of people from poorly vaccinated into highly vaccinated countries. This, however, is also unlikely to occur as public health authorities are already mandating testing and vaccination of immigrants as a prerequisite for entering the country
23 In case of CoV, there is no evidence that cytotoxic ‘one-size-fits-all’ T memory cells are generated 24 ‘Similar’ relates to pandemics of other acute self-limiting respiratory diseases (e.g., Influenza).
Author: G. Vanden Bossche, DVM, PhD March 2022
33
3. Continued evolution of the virus into a highly infectious and more virulent variant, thereby shifting VOCs (Variants of Concern) into VOHCs (Variants of High Consequence) that cause high rates of severe disease and mortality among individuals suffering from innate immune suppression, many of whom would be part of the vaccinated population. It’s only when that happens that the shrunk reservoir of healthy unvaccinated individuals will be able to provide sufficient sterilizing immunity to enable herd immunity.
Unless a large-scale antiviral program is immediately implemented in highly vaccinated countries, the increasing immune pressure exerted on Omicron’s pathogenicity will drive natural selection and propagation of new SC-2 variants (Newcos) that – in comparison to Omicron - will gain a tremendous competitive advantage on different fronts (full resistance to the vaccines resulting in enhanced infectiousness, transmissibility and virulence) and in all segments of the population that find their innate immune effector capacity suppressed, especially as a result of vaccination. C-19 vaccination not only suppresses the functionality of innate polyreactive Ab responses, which besides their protection from CoV also protect from other enveloped glycosylated viruses, but now also promotes viral infectiousness
25
since the potentially neutralizing vaccinal Abs have become subject to viral resistance . Since enhancing
vaccinal Abs are now causing strong immune pressure on viral virulence in highly vaccinated populations, enhanced infectiousness (ADEI) is paving the way for new escape mutants that will promote ADED. Vaccination against Omicron will parallel the effect of natural exposure to Omicron in that both will predominantly lead to a recall of enhancing anti-NTD Abs. Vaccinees who are at the highest risk of contracting severe disease are those who got vaccinated prior to natural exposure. Oncevaccinated, their innate immune cells may no longer be ‘trainable’ because of the prolonged suppressive effect of enhancing vaccinal Abs directed at the conserved antigenic site on S-NTD. These Abs will likely be boosted on regular occasions by the highly infectious circulating variant. But even additional booster injections with the current C-19 vaccines are only going to further raise the anti-NTD Ab titers and are, therefore, equally prone to promoting selection and expansion of ADED-enabling Newcos.
This sobering but truly scientific perspective is not even mentioning the many concerns raised in regard of the potential health consequences caused by long-lived suppression of immune recognition of self- like glycans that are expressed on host cells infected with other viruses (e.g., Influenza) or host cells that are pathologically altered by a non-infectious disease (e.g., cancer cells).
Why would vaccination with a live (attenuated) virus at the beginning of this pandemic (i.e., in an immunologically naïve population) not have had the same catastrophic prognosis?
Whereas high titers of neutralizing anti-S Abs (e.g., induced by modern vaccines) provide sterilizing immunity, suboptimal anti-S Abs that result from immunization during a pandemic will cause dominant propagation of more infectious immune escape variants and hence, lead to ever increasing titers of infection-enhancing Abs in the population. These Abs are to be considered a type of ‘pseudo-immunity’
25 Resistance to anti-RBM Abs rarely occurs in individuals who develop anti-S Abs as a result of natural disease because i) the anti-RBM Abs are a better match to the S antigen on the circulating variant than to the S antigen of the vaccine and ii) a natural immune response involves activation of the innate immune system prior to generation of anti-S Abs. The former will remove most of the viral load before high concentrations of anti-S Abs are reached.
Author: G. Vanden Bossche, DVM, PhD March 2022
34
in that they momentarily ‘paralyze’ the virus but cannot kill/ eliminate it. In the absence of pre-existing, neutralizing anti-S Abs, the best option for reaching herd immunity (during a pandemic) is to rely on trained innate immunity, potentially complemented with naturally acquired immunity. Genetically stable, live attenuated SC-2 could have contributed to training people’s innate immunity without driving immune escape. Of course, live attenuated vaccines are always at risk of causing (severe) disease in immunocompromised individuals.
How should a pandemic of an acute, self-limiting viral infection be monitored from a public health viewpoint?
The only way to reliably monitor the evolution of a pandemic is by measuring the evolution of the viral infection rate in the population. At this aim, standardized serological assays can be used that detect Abs against different assay targets (i.e., nucleocapsid and spike) to identify the proportion of vaccinated (presence of anti-spike antibodies only) and naturally infected individuals (presence of anti-nucleocapsid and anti-spike antibodies) [https://www.ecdc.europa.eu/sites/default/files/documents/Considerations- for-the-use-of-antibody-tests-for-SARS-CoV2-first-update.pdf]. As many SC-2 infections are now causing mild to moderate symptoms, population-level serology could be restricted to individuals who present with overt signs of C-19 disease; the assay should be repeated after 2 weeks to detect seroconversion. Itdoesn’t make any sense to look at the degree of disease or the level of shedding of those who got infected because a reduction in the severity of disease or level of shedding may even be associated with a higher level of viral infectiousness. Since a pandemic is a dynamic and evolutionary event that comes and goes in cyclic waves, it doesn’t make any sense either to look at snapshots of the infection rate taken at a particular point in time. To evaluate the success of any intervention, infection rates should be monitored over several weeks or months in order to evaluate whether the frequency and intensity of the waves of (measured) infection have diminished.
Conclusion
Mass vaccination has prevented a sound balance between viral infectiousness and natural immunity that would normally have developed during a natural pandemic as an overall trait of evolution enabling host populations to effectively control viral infection and transmission while leaving the virus a chance to perpetuate. To drive the virus into endemicity and maintain a such sound equilibrium between viral infectivity and population-level immunity, natural immunity is key as it is the only way to achieve herd immunity during a pandemic.
Whereas a natural pandemic naturally results in herd immunity, a pandemic that is disturbed by mass vaccination campaigns that are unable to cut the chain of viral transmission will eventually enable the virus to fully resist the vaccine-induced immune response. As a result of mounting population-level immune pressure on viral infectiousness (i.e., caused by vaccinal anti-RBD Abs), the virus will in a first step escape from the potentially neutralizing Abs and rise its level of infectiousness (ADEI). This has now translated in the dominant circulation of Omicron, which is highly infectious and largely resistant to potentially neutralizing vaccinal Abs. As a result of the increasing immune pressure that highly
Author: G. Vanden Bossche, DVM, PhD March 2022
35
vaccinated populations are now exerting on C type lectin-mediated viral ‘trans infectiousness’ (i.e., caused by non-neutralizing, ‘enhancing’ anti-NTD Abs), the virus will in a next step most likely evolve to also increase its virulence, thereby causing a dramatic rise in cases of severe disease (ADED) and death in vaccinees. As the mechanism of enhancement of infection and disease are mediated by binding of non-neutralizing Abs directed at a conserved site on the spike protein, the occurrence of ADEI and ADED will be particularly pronounced in ‘highly vaccinated- highly boosted’ populations exposed to a SC-2 variant that is largely resistant to vaccinal Abs that potentially inhibit viral infection (i.e., virus- neutralizing Abs). In the non-vaccinated, however, Omicron is boosting instead of compromising their innate immune defense against CoV, including all current and future variants. The type of mutations that the upcoming Newco variants are likely to incorporate to adapt to the immune pressure that highly vaccinated populations are now placing on the virulence/ pathogenicity of the virus (i.e., O-glycosite mutations) are likely to cause steric hindrance to both viral entry and trans infection in the non- vaccinated for lack of ‘enhancing’ Abs. This part of the population would, therefore, be spared from enhanced susceptibility to ADEI and ADED. Given the intrinsic debilitation of viral infectiousness and pathogenicity, even the more vulnerable among the unvaccinated would be less likely to contract severe disease upon viral exposure whereas they would be more likely to develop broadly cross-protective Abs. To restore a sound balance that benefits both the viral and the human population, it is paramount that either the viral infectious pressure or population-level immune pressure gets dramatically reduced. As both have become intrinsically linked in a highly vaccinated population, it suffices to either lower the infectious pressure or the immune pressure to reach that goal. Lowering the infectious pressure in highly vaccinated populations could only be achieved by mankind conducting large scale antiviral chemoprophylaxis campaigns; if man fails to do so, there is no doubt that the virus will take care of lowering the immune pressure in these populations.
Author: G. Vanden Bossche, DVM, PhD March 2022
36
Figures
Fig. 1: Case rates (underreported!) in all highly vaccinated countries (not India) remain high, with more or less strong fluctuations that clearly remain above the baseline
Author: G. Vanden Bossche, DVM, PhD March 2022
37
RT (ACE dependent)
LRT (ACE
independent)
neutralizingAbs to varia le
inverte
reg la on
non neutralizing Abs to conserve an NTD epitopes: ADEI
(localized infec on)
x
mild)
an
RBD epitopes ADII
cross
nhanced resistance to neutrali in an s
(e.g.,Omicron:enhancedresistance,moreinfec ous
Conserved across di erent SC variants
Inverted crossregula on relates to a conforma onal change in a variable RBD domain causing enhanced or impeded immune recogni on of the conserved NTD site
LRT: lower respiratory tract RT: upper respiratory tract
ADEI: Ab Dependent Enhancement of Infec on ADII: Ab Dependent Inhibi on of Infec on
Fig. 2: Enhanced resistance of a highly infectious SC-2 variant to neutralizing anti-RBD Abs is prone to causing ADEI while dampening viral pathogenicity/ virulence by hampering trans infection
an
cross
(localized infec
on)
to varia le RBD epitopes
ADII
inverte
reg la on
naturall ac uired anS s
rained innate polreace
RT (ACE dependent) neutralizingAbs
non neutralizing Abs to conserve an NTD epitopes: ADEI
x
mild)
LRT (ACE independent)
non neutralizing
an NTD Abs
LRT: lower respiratory tract RT: upper respiratory tract
ADEI: Ab Dependent Enhancement of Infec on ADII: Ab Dependent Inhibi on of Infec on
nhanced resistance to neutrali in an
s
(e.g., Omicron: enhanced resistance, more infec
ous
Conserved across di erent SC variants
Inverted cross regula on relates to a conforma onal change in a variable RBD domain causing enhanced or impeded immune recogni on of the conserved NTD site
Fig. 3: Innate polyreactive Abs compete with non-neutralizing anti-NTD Abs for binding to SC-2 virions. The higher the affinity of the innate Abs (training!) and the lower the affinity of the vaccinal anti-NTD Abs, the more effectively the innate immune system will eliminate SC-2 variants. Sera from vaccinated individuals have poor virus-neutralizing capacity and are, therefore, likely to have a relatively high infection-enhancing capacity. The latter is mediated by high-affinity anti-NTD Abs, which are continuously boosted during a pandemic and cannot be outcompeted by untrained innate Abs
Author: G. Vanden Bossche, DVM, PhD March 2022
38
trans
fusion
fusion
trans
infec on
trans
(systemic disease)
infec on
trans
(systemic disease)
Trained innate immunity
Mass C 19 vaccina
on Omicron
(resistance to neutralizing an RBDvaccinalAbs)
enhancing an NTD Newco ADED vaccinal Abs
Newco
ADEI (mild disease)
!
Largescalean viral chemoprophylaxis
Fig. 4: Consequences of C-19 mass vaccination during a SC-2 pandemic. Resistance of the circulating immune escape to potentially neutralizing vaccinal Abs inevitably leads to a high incidence of ADEI and ultimately to ADEI-mediated ADED in highly vaccinated populations. Because high titers of enhancing anti-NTD Abs outcompete innate IgMs for binding to SC-2, a high prevalence of elevated enhancing anti-NTD Ab titers in the population causes population-level suppression of innate Ab- mediated immunity and, therefore, prevents herd immunity. As lack of herd immunity will allow the chain of viral transmission to continue, the evolutionary dynamics of the virus will not be halted until the contribution of individuals with high infection- enhancing titers is dramatically reduced. To avoid a such disastrous development of the current pandemic, it is paramount to cut the chain of viral transmission by deploying large scale antiviral chemoprophylaxis campaigns in highly vaccinated populations or by implementing an immunization strategy that fosters a critical component of people’s first line of immune defense that cannot be outcompeted by Abs (i.e., innate/ natural killer cells). The circulating virus itself will fail to train innate immune effector cells in vaccinees as it will continuously recall the enhancing anti-NTD Abs that outcompete the polyreactive IgMs. The numbers (1-6) indicate the sequence of the immunopathogenic events.
Author: G. Vanden Bossche, DVM, PhD March 2022
39
Omicron (resistance to enhancing an NTD vaccinal Abs
Enhancedtransinfec on ost cell
ACE
RRBBDD
NTD NTD
Enhancing Ab
ACE
RBD
NTD NTD
DC
x
Enhancedinfec on
ost cell ACE ACE
RBD RBD
NTD NTD NTD NTD
Enhancing Ab
Ab: An body
ACE : Angiotensin conver ng enzyme
DC: Dendri c Cell
NTD: N terminal domain on spike protein
RBD: Receptor binding domain on spike protein
Fig. 5: Right panel: Putative conformational arrangement of spike protein (RBD + NTD) on free virions of a Newco variant. The open RBD state is induced upon binding of enhancing Abs to a specific site on NTD. Multivalent binding enables binding of the RBD to the ACE2 receptor. The opening of RBD and, therefore, ADEI would not be hampered by its additional O-glycosylation of predicted O-glycosylation sites on the RBD (glycans indicated by black horizontal bars). Left panel: The RBD of S expressed on virions that are tethered to the surface of migrating DCs adopts a closed conformation, allowing its O-glycosylation patch to shield the specific conserved infection-enhancing domain within NTD and thereby prevent infection-enhancing Abs from binding and inducing conformational changes that would hamper fusogenic rearrangement of S that is normally mediated by a ganglioside-binding domain on S-NTD. In this way, O-glycosylation (together with compensatory amino acid mutations in the variable part of NTD) could prevent inhibition of trans infection from migratory DCs to host cells.
Author: G. Vanden Bossche, DVM, PhD March 2022
40
RT (ACE
inverte
reg la on
dependent)
LRT (ACE
independent)
neutralizingAbs to varia le
an RBD epitopes ADII
cross
non neutralizing Abs x to conserve an NTD
epitopes: ADEI (localized infec on)
inverte cross reg la on
nhanced resistance to neutrali in an s
(Omicron:moreinfec ous mild)
Conserved across di
Inverted cross regula on relates to a conforma onal change in a variable RBD domain causing enhanced or impeded immune recogni on of the conserved NTD site
erent SC variants
l cos la on
via non neutralizingAbs to
varia le an
NTD epitopes
LRT: lower respiratory tract RT: upper respiratory tract
ADED: Ab Dependent Enhancement of Disease ADEI: Ab Dependent Enhancement of Infec on ADII: Ab Dependent Inhibi on of Infec on
Newco variant: fullyresistant, highlyinfec ous virulence
Fig. 6: Large scale vaccination with C-19 vaccine during a pandemic of more infectious immune escape variants promotes the propagation of immune escape variants (e.g., Omicron) that resist anti-RBD Abs and generates a high prevalence of elevated enhancing anti-NTD Ab titers in the population. This causes a high propensity to ADEI among vaccinees (i.e., enhanced susceptibility to infection) and promotes the propagation of immune escape variants (e.g., the predicted Newco variants) that are likely to use O-glycosylation at the N-terminal end of the RBD to not only resist anti-RBD Abs but also enhance anti-NTD Abs. O-glycosylation at predicted sites on the RBD would optimize inhibition of virus neutralization while blocking anti-NTD Ab- mediated inhibition of trans infection and, therefore, promote anti-NTD Ab-mediated trans fusion between infected and non- infected cells in the LRT or distant organs while enabling ADEI-mediated ADED. Enhanced O-glycosylation of S will, therefore, lead to an increased incidence of ADED among vaccinees.
Author: G. Vanden Bossche, DVM, PhD March 2022
41
trans
fusion
trans
infec on
(systemic disease)
Fig. 7: The evolutionary dynamics of emerging Newco variants are expected to lead to an exponential rise of hospitalizations (i.e., severe morbidity) and mortality rates in parallel with their exponential expansion in prevalence. X: indicates start of dominance of next Newco variant; dashed lines indicate ‘valley of fitness’. (VOF); •: indicates start of selection of next Newco variant
Author: G. Vanden Bossche, DVM, PhD March 2022
revalence of Newco
Newco Newco
Newco Newco 1
O1OO
Attachment
I. About glycosylation of SC-2
I gained important insights on glycosylation of coronavirus spike protein (including S from SC-2) as well as on the interaction of SC-2 glycans with C-type lectins and their potential to modulate SC-2 infectiousness from the following excellent reviews:
https://pubmed.ncbi.nlm.nih.gov/32178593/ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7199903/ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7253482/ https://www.frontiersin.org/articles/10.3389/fmolb.2021.629873/full https://academic.oup.com/glycob/article/28/7/443/4951691 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7863934/pdf/ijms-22-00992.pdf https://pubmed.ncbi.nlm.nih.gov/32178593/ https://pubs.acs.org/doi/pdf/10.1021/acscentsci.0c01056
It has been repeatedly reported that glycans play a role in occluding specific regions on glycoproteins that are exposed and are, therefore, vulnerable to immune recognition. Site-specific glycosylation analysis has revealed that the glycan shield of SC-2 spike protein is consistent with other coronaviruses and similarly exhibits numerous vulnerabilities throughout the glycan shield, including the part of NTD that is recognized by infection-enhancing Abs (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7253482/; https://pubmed.ncbi.nlm.nih.gov/32366695/). The mannose residues comprised within the vast majority of mannosylated N-linked glycans that decorate SC-2 S protein are important moieties to interact with cell surface attachment factors, like glycosaminoglycans (GAGs) and sialic acid-containing oligosaccharides on the surface of target cells (https://www.pnas.org/doi/epdf/10.1073/pnas.1712592114;https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7112261/; https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7278709/;https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7128678/) before binding to the angiotensin- converting enzyme 2 (ACE2) receptor (https://www.nature.com/articles/s41580-021-00418-x.pdf).
C-type lectins (DC-SIGN, L-SIGN or SIGLEC1) on certain host cells that only express ACE2 at very low levels, such as dendritic cells or endothelial and alveolar epithelial cells, can also serve as attachment factors for oligomannosylated N-linked glycans to facilitate ACE2-dependent trans infection or ACE2- independent trans fusion, respectively (see below under III).
II. About O-glycosylation of SC-2
O-glycans have also been observed on some viral proteins and have been suggested to play roles in the biological activity of viral proteins (https://academic.oup.com/glycob/article/28/7/443/4951691; https://www.nature.com/articles/s41591-020-0820-9). In regard of O-glycosylation of SC-2 spike protein, the best summary on the current status can probably be found in a review published by X. Zhao et al. ( https://www.frontiersin.org/articles/10.3389/fmolb.2021.629873/full) stating the following:
Author: G. Vanden Bossche, DVM, PhD March 2022
43
“In contrast to the consistent results of N-linked glycosylation, different groups have reported different O-linked glycosylation patterns of S protein depending on different protein expression systems and detection methods employed. Shajahan et al. reported a high level of O-glycosylation of S1 and S2 when expressed independently and detected O-glycosylation at sites Thr323 and Ser325 on the S1 subunit of the S protein (Shajahan et al., 202026). However, other two reports detected low occupancy at most sites
27 28
of O-glycan modification using S trimer for analysis (Watanabe et al ., 2020; Zhao et al., 2020 ). One
possible explanation for this discrepancy is that the S protein could undergo different types of glycosylation at different conformations or oligomeric states. In addition, Andersen et al. predicted a unique O-linked glycosylation pattern flanking the furin cleavage site (Andersen et al., 202029), and glycosylation around this cleavage site is thought to regulate the activation of the S protein. Sanda et al. confirmed this O-glycosylation near the furin cleavage site (T678) using MS-based methods; in addition, they identified another eight O-glycopeptides (Sanda et al., 202030). The functional role of most of the O- linked glycosylation is not fully understood.”
An asparagine residue can accept an oligosaccharide only if the residue is part of an Asn-X-Ser or Asn-X- The sequence, in which X can be any residue except proline (https://cshperspectives.cshlp.org/content/5/8/a013359). In contrast, there are no conserved protein sequence motifs for general or isoform-specific O-glycosylation, and therefore it is much more difficult to predict this modification (https://www.jbc.org/article/S0021-9258(20)51541-X/fulltext;https://academic.oup.com/glycob/article/28/7/443/4951691).
Until now, mutations in dominant variants, including Omicron, have not been reported to affect glycosylation sites containing oligomannose-type glycans (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7253482/). This finding seems to indicate that the glycosylation sites are generally spared by selective pressure, suggesting that they are essential and sufficient for SC-2 infectivity. However, it has been shown that mechanisms of in vitro escape of SC- 2 from highly neutralizing COVID-19 convalescent plasma include the insertion of a new glycan sequon in the N-terminal domain of the spike protein, which leads to complete resistance to neutralization https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7781313/
III. About the role of C-type lectins in the pathobiology of SC-2 infections
C-type lectin receptors (e.g., DC-SIGN/L-SIGN/ LSECtin), expressed on several different types of host cells recognize mannosylated N-glycans (i.e., high mannose type and complex N-glycans) and O-glycan moieties present on SC-2 S protein. Depending on the cell type they decorate and their level of cell
26 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7239183/ 27 https://pubmed.ncbi.nlm.nih.gov/32366695/
28 https://www.sciencedirect.com/science/article/pii/S1931312820304571 29 https://www.nature.com/articles/s41591-020-0820-9
30 https://www.biorxiv.org/content/10.1101/2020.07.05.187344v1
Author: G. Vanden Bossche, DVM, PhD March 2022
44
surface expression , C-type lectins may facilitate cis or trans infection to enable ACE2-mediated viral entry into host cells (https://www.nature.com/articles/s41590-021-01091-0.pdf).
Author: G. Vanden Bossche, DVM, PhD March 2022
45
.)

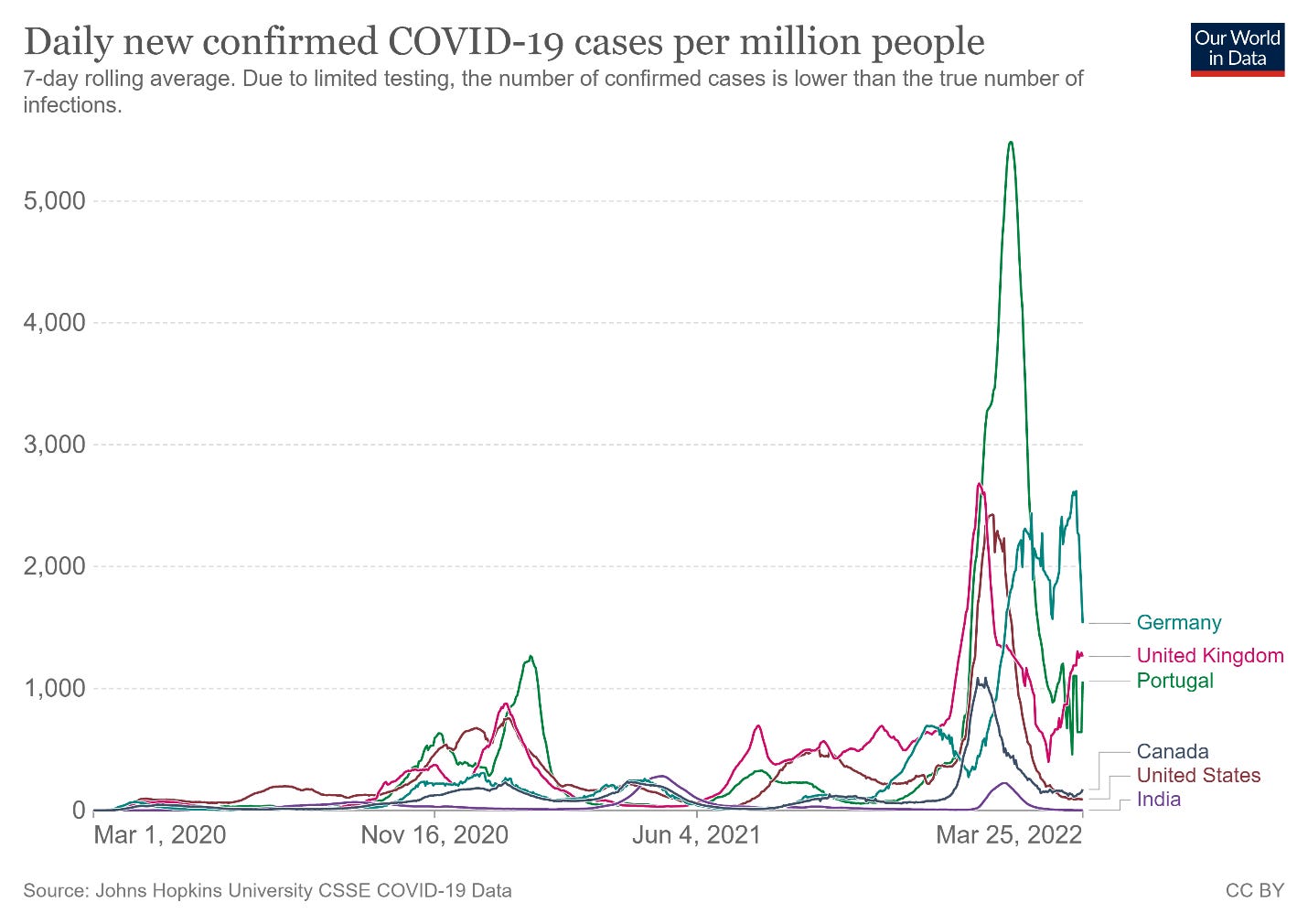











How protected are we if we are unvaxxed and had a solid sickness with Omicron against future variants?